Final ID: Sa2034
Associations Between Chronic Kidney Disease and Inflammatory Biomarkers in the Genetic Epidemiology Network of Arteriopathy Cohort
Abstract Body (Do not enter title and authors here): Background: Chronic kidney disease (CKD) has been linked to elevated inflammatory biomarkers, yet few studies have evaluated these associations using iothalamate-based measures of kidney function, highlighting the need for further research.
Research question: Is CKD associated with elevated inflammatory markers when defined by measured glomerular filtration rate (mGFR) and urinary albumin-to-creatinine ratio (UACR)?
Methods: Participants from the Genetic Epidemiology Network of Arteriopathy (GENOA) cohort were included if they had data available for at least one inflammatory marker at visit 2. 17 inflammatory markers were assessed, including C-reactive protein (CRP), interleukin-6 (IL-6), IL-18, tumor necrosis factor receptors 1 and 2 (TNFR1, TNFR2), serum amyloid A, intercellular and vascular adhesion molecules (ICAM, VCAM), E-selectin, P-selectin, monocyte chemoattractant protein (MCP), myeloperoxidase (MPO), receptor for advanced glycation end products (RAGE), matrix metalloproteinases 2 and 9 (MMP-2, MMP-9), and tissue inhibitors of metalloproteinases 1 and 2 (TIMP-1, TIMP-2). Kindey function was assessed using the urinary clearance of iothalamate. CKD was defined as mGFR < 60 mL/min/1.73 m2 or UACR ≥ 30 mg/g. To further assess whether associations persisted without albuminuria, we also defined CKD solely by mGFR < 60 mL/min/1.73 m2. Generalized estimating equations (GEE) were used to assess associations between CKD status and inflammatory markers, accounting for familial clustering. Exponentiated beta coefficients from GEE models were used to present geometric mean (GM) ratios of each biomarker by CKD status, adjusted for demographics, lifestyle factors, cardiovascular risk factors, and medication use.
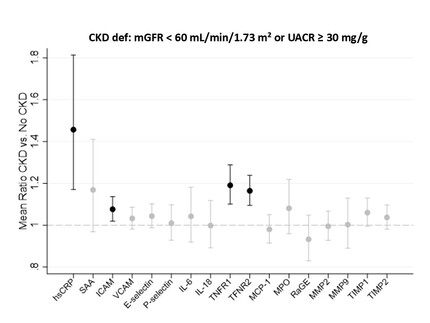
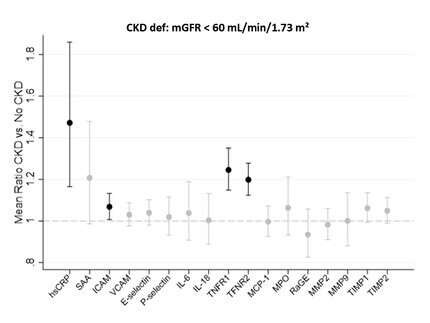
Results: Among 1,010 participants (mean age 61 ± 10 years; 67% women; 48% Black adults), 207 were classified as having CKD. After adjusting for potential confounders, individuals with CKD had significantly higher levels of hsCRP, VCAM, TNFR1, and TNFR2 compared to those without CKD (GM ratios > 1; p < 0.05), while the remaining inflammatory markers showed no significant differences (Figure 1). Importantly, these elevations remained significant when CKD was defined by mGFR alone (Figure 2).
Conclusion: Our findings suggest that CKD, defined by mGFR, is associated with specific inflammatory biomarkers, underscoring the need for mechanistic studies to investigate these associations.
Research question: Is CKD associated with elevated inflammatory markers when defined by measured glomerular filtration rate (mGFR) and urinary albumin-to-creatinine ratio (UACR)?
Methods: Participants from the Genetic Epidemiology Network of Arteriopathy (GENOA) cohort were included if they had data available for at least one inflammatory marker at visit 2. 17 inflammatory markers were assessed, including C-reactive protein (CRP), interleukin-6 (IL-6), IL-18, tumor necrosis factor receptors 1 and 2 (TNFR1, TNFR2), serum amyloid A, intercellular and vascular adhesion molecules (ICAM, VCAM), E-selectin, P-selectin, monocyte chemoattractant protein (MCP), myeloperoxidase (MPO), receptor for advanced glycation end products (RAGE), matrix metalloproteinases 2 and 9 (MMP-2, MMP-9), and tissue inhibitors of metalloproteinases 1 and 2 (TIMP-1, TIMP-2). Kindey function was assessed using the urinary clearance of iothalamate. CKD was defined as mGFR < 60 mL/min/1.73 m2 or UACR ≥ 30 mg/g. To further assess whether associations persisted without albuminuria, we also defined CKD solely by mGFR < 60 mL/min/1.73 m2. Generalized estimating equations (GEE) were used to assess associations between CKD status and inflammatory markers, accounting for familial clustering. Exponentiated beta coefficients from GEE models were used to present geometric mean (GM) ratios of each biomarker by CKD status, adjusted for demographics, lifestyle factors, cardiovascular risk factors, and medication use.
Results: Among 1,010 participants (mean age 61 ± 10 years; 67% women; 48% Black adults), 207 were classified as having CKD. After adjusting for potential confounders, individuals with CKD had significantly higher levels of hsCRP, VCAM, TNFR1, and TNFR2 compared to those without CKD (GM ratios > 1; p < 0.05), while the remaining inflammatory markers showed no significant differences (Figure 1). Importantly, these elevations remained significant when CKD was defined by mGFR alone (Figure 2).
Conclusion: Our findings suggest that CKD, defined by mGFR, is associated with specific inflammatory biomarkers, underscoring the need for mechanistic studies to investigate these associations.
More abstracts on this topic:
Arteriovenous fistula creation results in cardiac dysfunction and remodeling in a uremic pig model
Kane Jamie, Collins Jeremy, Lee Timmy, Misra Sanjay, Singh Prabh, Kilari Sreenivasulu, Baranwal Gaurav, Naskar Atanu, Montonye Dan, Lutgens Esther, Wang Ying, Negm Ahmed
Activated T cells from Bph/2 Mice Have an Attenuated Cytokine Response to a Polyclonal T Cell Activator Compared to T cells from Bpn/3 MiceRockwell Cheryl, Dattmore Devon, Mcdonald Paiton, Chowdhury Afrin, Awali Saamera, Boss Allison, Sather Lisa, Lauver Adam