Final ID: Sa2033
Chronic Kidney Disease with Inflammation and Incident Coronary Heart Disease in Black Adults from the Jackson Heart Study
Abstract Body (Do not enter title and authors here): Background:
Inflammation and chronic kidney disease (CKD) increase the risk of coronary heart disease (CHD), which disproportionately affects Black adults. However, it remains unclear whether the coexistence of inflammation and CKD confers a greater risk than either condition alone.
Research Question:
Does the coexistence of inflammation and CKD confer a higher risk of incident CHD compared to either condition alone?
Methods:
We included baseline data (2000–2004) from Jackson Heart Study participants with available measurements of inflammation, defined as high-sensitivity C-reactive protein (hsCRP) ≥ 3 mg/L, and chronic kidney disease (CKD), defined as estimated glomerular filtration rate (eGFR) < 60 mL/min/1.73m2 (CKD 2021 EPI equation), and without CHD. Participants were classified into four groups: no CKD and no inflammation (reference group), inflammation without CKD, CKD without inflammation, and CKD with inflammation and followed through 2016 for incident CHD. Cox proportional hazards models were used to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) for incident CHD events defined as adjudicated probable or definite myocardial infarction (MI), fatal MI, or a history of cardiac procedures including percutaneous coronary intervention or coronary artery bypass grafting. The fully adjusted model included covariates for age, sex, systolic blood pressure, antihypertensive medications, diabetes, smoking, alcohol, physical activity, statins, total cholesterol, LDL-C, and HDL-C.
Results:
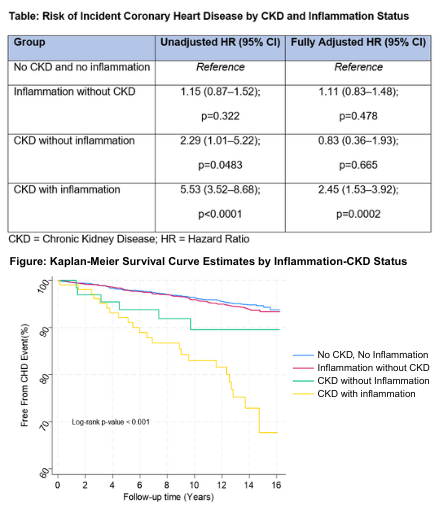
Among 4,073 participants (mean age 53.9±12.8 years; 64.3% women), 2,140 (52.5%) had no CKD and no inflammation, 1,761 (43.2%) had inflammation without CKD, 66 (1.6%) had CKD without inflammation, and 106 (2.6%) had CKD with inflammation. Over a median follow-up of 13.8 years, the unadjusted models showed that CHD risk was highest in the CKD with inflammation group (HR 5.53, 95% CI 3.52–8.68). Risk was also elevated in those with CKD without inflammation (HR 2.29, 95% CI 1.01–5.22), but not in those with inflammation without CKD (HR 1.15, 95% CI 0.87–1.52). After adjustment for covariates, only the CKD with inflammation group remained significantly associated with incident CHD (HR 2.45, 95% CI 1.53–3.92).
Conclusion:
Black adults with concomitant inflammation and CKD have a significantly higher risk of incident CHD compared to those with either condition alone, highlighting the need for intensive management and the potential role of novel anti-inflammatory therapies.
Inflammation and chronic kidney disease (CKD) increase the risk of coronary heart disease (CHD), which disproportionately affects Black adults. However, it remains unclear whether the coexistence of inflammation and CKD confers a greater risk than either condition alone.
Research Question:
Does the coexistence of inflammation and CKD confer a higher risk of incident CHD compared to either condition alone?
Methods:
We included baseline data (2000–2004) from Jackson Heart Study participants with available measurements of inflammation, defined as high-sensitivity C-reactive protein (hsCRP) ≥ 3 mg/L, and chronic kidney disease (CKD), defined as estimated glomerular filtration rate (eGFR) < 60 mL/min/1.73m2 (CKD 2021 EPI equation), and without CHD. Participants were classified into four groups: no CKD and no inflammation (reference group), inflammation without CKD, CKD without inflammation, and CKD with inflammation and followed through 2016 for incident CHD. Cox proportional hazards models were used to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) for incident CHD events defined as adjudicated probable or definite myocardial infarction (MI), fatal MI, or a history of cardiac procedures including percutaneous coronary intervention or coronary artery bypass grafting. The fully adjusted model included covariates for age, sex, systolic blood pressure, antihypertensive medications, diabetes, smoking, alcohol, physical activity, statins, total cholesterol, LDL-C, and HDL-C.
Results:
Among 4,073 participants (mean age 53.9±12.8 years; 64.3% women), 2,140 (52.5%) had no CKD and no inflammation, 1,761 (43.2%) had inflammation without CKD, 66 (1.6%) had CKD without inflammation, and 106 (2.6%) had CKD with inflammation. Over a median follow-up of 13.8 years, the unadjusted models showed that CHD risk was highest in the CKD with inflammation group (HR 5.53, 95% CI 3.52–8.68). Risk was also elevated in those with CKD without inflammation (HR 2.29, 95% CI 1.01–5.22), but not in those with inflammation without CKD (HR 1.15, 95% CI 0.87–1.52). After adjustment for covariates, only the CKD with inflammation group remained significantly associated with incident CHD (HR 2.45, 95% CI 1.53–3.92).
Conclusion:
Black adults with concomitant inflammation and CKD have a significantly higher risk of incident CHD compared to those with either condition alone, highlighting the need for intensive management and the potential role of novel anti-inflammatory therapies.
More abstracts on this topic:
A multi-proteomic Risk Score Predicts Adverse Cardiovascular Outcomes in Patients with Angina and Non-obstructive Coronary Artery Disease
Huang Jingwen, Lodhi Rafia, Lodhi Saleha, Eldaidamouni Ahmed, Hritani Wesam, Hasan Muhammet, Haroun Nisreen, Quyyumi Arshed, Mehta Puja, Leon Ana, Ko Yi-an, Yang Huiying, Medina-inojosa Jose, Ahmed Taha, Harris Kristen, Alkhoder Ayman, Al Kasem Mahmoud
A Shocking Postpartum CourseWozniak Phillip, Grodzinsky Anna