Final ID: MP360
Association of Inflammatory Hypertension with Left Ventricular Hypertrophy in Black Adults from the Genetic Epidemiology Network of Arteriopathy Study
Abstract Body (Do not enter title and authors here): Background: Hypertension and systemic inflammation are independently associated with adverse cardiovascular outcomes. While hypertension is a known risk factor for left ventricular (LV) hypertrophy, the role of inflammation in LV structural changes remains unclear. It is also uncertain whether concomitant inflammation and hypertension ("inflammatory hypertension") exacerbate LV hypertrophy.
Research Question: Is inflammatory hypertension associated with increased LV mass index (LVMI) compared to hypertension without inflammation?
Methods: We analyzed baseline data from Black adults enrolled in the Genetic Epidemiology Network of Arteriopathy (GENOA) cohort in Jackson, Mississippi. Inflammation was defined by high sensitivity C-reactive protein (hsCRP) >3 mg/L, and hypertension as systolic blood pressure (SBP) >130 mmHg. Participants were classified into four groups: noninflammatory-normotensive (reference group), noninflammatory-hypertensive, inflammatory-normotensive, and inflammatory-hypertensive. The primary outcome was LVMI, assessed by echocardiography. Associations between groups and LVMI were evaluated using generalized estimating equations to account for familial clustering and adjusted for covariates including age, sex, education, smoking status, body mass index, number of antihypertensive medications, statin use, cholesterol, and diabetes.
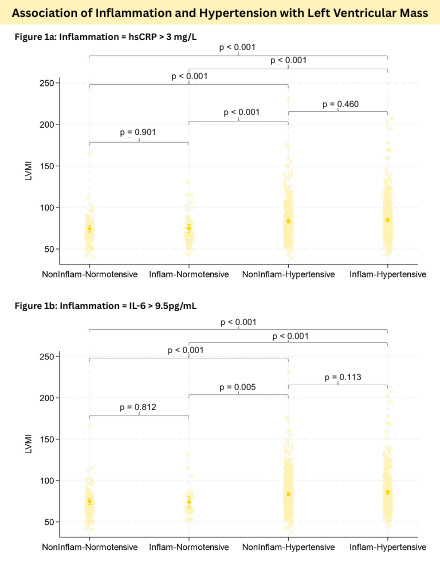
Results: Among 1,027 participants (mean age 64 ± 8.5 years; 71% women), baseline LVMI differed by inflammation-hypertension status. Compared with the LVMI in noninflammatory-normotensive cohort (n=108; 74.5 g/m2 [70.4–78.6]), significantly higher LVMI was observed in noninflammatory-hypertensive (n=343; 83.6 g/m2 [81.3–85.9], p<0.001) and inflammatory-hypertensive groups (n=497; 84.7 g/m2 [82.8–86.7], p<0.001). There was no statistically significant difference between inflammatory-hypertensive and noninflammatory-hypertensive groups (84.7 vs 83.6 g/m2)(p=0.460). The inflammatory-normotensive cohort also did not differ from the reference group (74.9 g/m2 [70.2–79.5], p=0.901). Secondary analyses using elevated IL-6 to define inflammation yielded similar findings (Figure 1).
Conclusion: In individuals with inflammatory hypertension, hypertension appears to be the primary driver of LV hypertrophy. Further studies in larger, diverse populations are needed to definitively evaluate the potential additive effect of inflammatory hypertension on LV remodeling.
Research Question: Is inflammatory hypertension associated with increased LV mass index (LVMI) compared to hypertension without inflammation?
Methods: We analyzed baseline data from Black adults enrolled in the Genetic Epidemiology Network of Arteriopathy (GENOA) cohort in Jackson, Mississippi. Inflammation was defined by high sensitivity C-reactive protein (hsCRP) >3 mg/L, and hypertension as systolic blood pressure (SBP) >130 mmHg. Participants were classified into four groups: noninflammatory-normotensive (reference group), noninflammatory-hypertensive, inflammatory-normotensive, and inflammatory-hypertensive. The primary outcome was LVMI, assessed by echocardiography. Associations between groups and LVMI were evaluated using generalized estimating equations to account for familial clustering and adjusted for covariates including age, sex, education, smoking status, body mass index, number of antihypertensive medications, statin use, cholesterol, and diabetes.
Results: Among 1,027 participants (mean age 64 ± 8.5 years; 71% women), baseline LVMI differed by inflammation-hypertension status. Compared with the LVMI in noninflammatory-normotensive cohort (n=108; 74.5 g/m2 [70.4–78.6]), significantly higher LVMI was observed in noninflammatory-hypertensive (n=343; 83.6 g/m2 [81.3–85.9], p<0.001) and inflammatory-hypertensive groups (n=497; 84.7 g/m2 [82.8–86.7], p<0.001). There was no statistically significant difference between inflammatory-hypertensive and noninflammatory-hypertensive groups (84.7 vs 83.6 g/m2)(p=0.460). The inflammatory-normotensive cohort also did not differ from the reference group (74.9 g/m2 [70.2–79.5], p=0.901). Secondary analyses using elevated IL-6 to define inflammation yielded similar findings (Figure 1).
Conclusion: In individuals with inflammatory hypertension, hypertension appears to be the primary driver of LV hypertrophy. Further studies in larger, diverse populations are needed to definitively evaluate the potential additive effect of inflammatory hypertension on LV remodeling.
More abstracts on this topic:
AI-Driven Electrocardiographic Detection and Subtyping of Hypertrophic Cardiomyopathy: A Deep Learning Approach Using 12-Lead ECGs
Soh Moon Seung, Yu Taehyung, Na Yeongyeon, Joo Sunghoon, Shin Joon-han
2 Dimensional Echocardiography versus 3 Dimentional Echocardiography to Assess Right Ventricular Function in Pulmonary Hypertension: A Systematic ReviewChaudhry Waleed Razzaq, Hajj Fatima, Bathula Satyamedha, Meghji Mohammed Askari, Pasupuleti Hemalatha, Kiyani Madiha, Shah Syeda Simrah, Neelakantan Ramaswamy Sanathanan, Mirzaeidizaji Nakisa, St. Jacques Jahnoy, Khan Khalil Ullah, Veluchamy Elakkiya, Jesse Joshanna