Final ID: MP67
Outcomes of Open Cardiac Surgery in Patients with Preoperative Iron Deficiency Anemia: A Propensity-Matched Multicenter Retrospective Analysis
Abstract Body (Do not enter title and authors here): Introduction:
Iron deficiency anemia (IDA) may adversely affect perioperative outcomes due to impaired oxygen delivery and reduced immune function. However, data on the specific impact of IDA on outcomes following open cardiac surgery is limited. Understanding this relationship could guide pre- and peri-operative optimization.
Objectives:
This study retrospectively compares postoperative complications and survival in IDA versus non-anemic patients who underwent open cardiac procedures.
Methods:
The TriNetX global federated health research network was used to retrieve data for patients who underwent any open cardiac surgery procedures with and without IDA. The IDA cohort included 117,325 patients from 69 centers whereas the non-IDA cohort retrieved data from 519,858 patients from 71 centers. Propensity matching was performed for age, gender, race, type 2 diabetes mellitus, nicotine dependence, chronic cardiovascular renal and hepatic comorbidities, procedure performed and prescribed medications to prevent any confounding. The primary outcomes were all cause mortality, sepsis, and major adverse cardiac events (MACE): a composite of cardiac mortality, non-fatal cerebrovascular events and non-fatal myocardial infarctions. Risk Difference with 95% confidence intervals was calculated using a two-proportion Z-test.
Results:
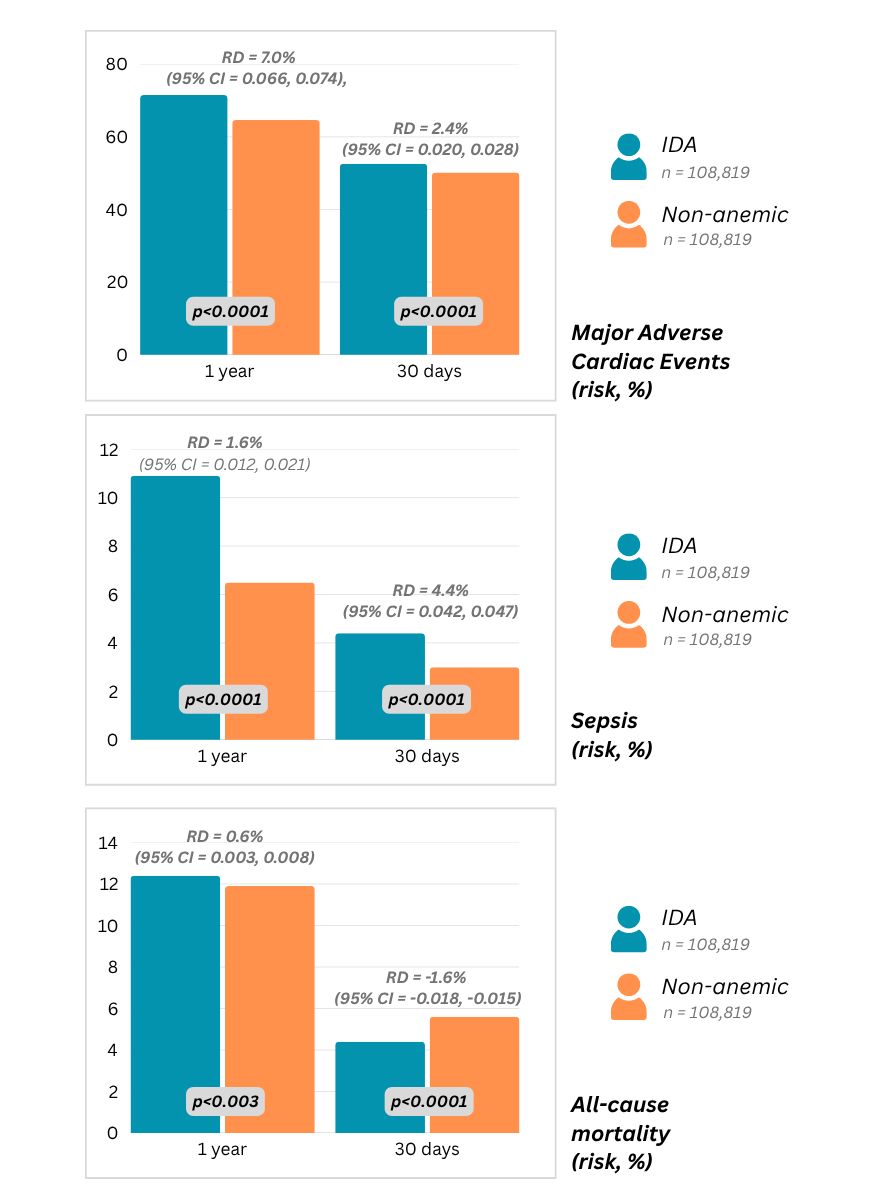
There were a total of 108,819 patients compared after propensity matching. MACE was significantly higher in patients with IDA at 30 days (RD = 2.4% (95% CI = 0.020, 0.028), p < 0.0001) and 1 year (RD = 7.0% (95% CI = 0.066, 0.074), p<0.0001). Sepsis incidence was also greater in patients with IDA at both time intervals. i.e. 30 days: (RD = 1.4% (95% CI = 0.012, 0.015), p<0.0001), 1 year: (RD = 4.4% (95% CI = 0.042, 0.047), p<0.0001). All-cause mortality at 30-days was higher in the control group (RD = -1.6% (95% CI = -0.018, -0.015), p<0.0001); however at 1 year it was greater in the IDA group (RD = 0.6% (95% CI = 0.003, 0.008), p<0.0001). Post-procedural cardiac complications at 30 days that were higher in patients with IDA included arrythmias (RD=0.6% (95% CI = -0.011, -0.002), p=0.003) and left ventricular failure (RD=0.3% (95% CI = 0.002, 0.004), p<0.0001).
Conclusion:
Preoperative IDA is linked to significantly higher rates of MACE, sepsis and late mortality following open cardiac surgery. These findings underscore the urgency of recognizing IDA as a modifiable risk factor to improve survival and recovery after open cardiac surgery.
Iron deficiency anemia (IDA) may adversely affect perioperative outcomes due to impaired oxygen delivery and reduced immune function. However, data on the specific impact of IDA on outcomes following open cardiac surgery is limited. Understanding this relationship could guide pre- and peri-operative optimization.
Objectives:
This study retrospectively compares postoperative complications and survival in IDA versus non-anemic patients who underwent open cardiac procedures.
Methods:
The TriNetX global federated health research network was used to retrieve data for patients who underwent any open cardiac surgery procedures with and without IDA. The IDA cohort included 117,325 patients from 69 centers whereas the non-IDA cohort retrieved data from 519,858 patients from 71 centers. Propensity matching was performed for age, gender, race, type 2 diabetes mellitus, nicotine dependence, chronic cardiovascular renal and hepatic comorbidities, procedure performed and prescribed medications to prevent any confounding. The primary outcomes were all cause mortality, sepsis, and major adverse cardiac events (MACE): a composite of cardiac mortality, non-fatal cerebrovascular events and non-fatal myocardial infarctions. Risk Difference with 95% confidence intervals was calculated using a two-proportion Z-test.
Results:
There were a total of 108,819 patients compared after propensity matching. MACE was significantly higher in patients with IDA at 30 days (RD = 2.4% (95% CI = 0.020, 0.028), p < 0.0001) and 1 year (RD = 7.0% (95% CI = 0.066, 0.074), p<0.0001). Sepsis incidence was also greater in patients with IDA at both time intervals. i.e. 30 days: (RD = 1.4% (95% CI = 0.012, 0.015), p<0.0001), 1 year: (RD = 4.4% (95% CI = 0.042, 0.047), p<0.0001). All-cause mortality at 30-days was higher in the control group (RD = -1.6% (95% CI = -0.018, -0.015), p<0.0001); however at 1 year it was greater in the IDA group (RD = 0.6% (95% CI = 0.003, 0.008), p<0.0001). Post-procedural cardiac complications at 30 days that were higher in patients with IDA included arrythmias (RD=0.6% (95% CI = -0.011, -0.002), p=0.003) and left ventricular failure (RD=0.3% (95% CI = 0.002, 0.004), p<0.0001).
Conclusion:
Preoperative IDA is linked to significantly higher rates of MACE, sepsis and late mortality following open cardiac surgery. These findings underscore the urgency of recognizing IDA as a modifiable risk factor to improve survival and recovery after open cardiac surgery.
More abstracts on this topic:
A Multi-centre, Randomized, Controlled Study of External CounterPulsation for Patients with Recent Atherosclerotic Stroke (SPA)
Xiong Li, Chen Xiangyan, Leung Howan, Zhu Lixia, Leung Thomas, Wong Lawrence
Anti-inflammatory regimen associated with reduced incidence of early homograft stenosis following the Ross procedureKhan Kathleen, Degraaff Dominique, Gray Mary Anne, Korukonda Samhita, Flodin Rachel, Degraaff Bret, Dhanekula Arjune, Deroo Scott, Burke Christopher