Final ID: Sa2085
Temporal Trends in Endocarditis-Related Mortality in Patients With Cardiac Device Complications in the United States, 1999–2023: A Joinpoint Regression Analysis
Abstract Body (Do not enter title and authors here): Background:
Cardiac devices such as prosthetic valves, coronary bypass grafts, and implantable hardware have improved survival but are associated with increased infection risk. Infective endocarditis (IE) remains a life-threatening complication of device-related infections. Despite advances in antimicrobial strategies and perioperative protocols, long-term national trends in endocarditis-related mortality with cardiac device complications remain under-characterized.
Methods:
Using the CDC WONDER Multiple Cause of Death database (1999–2023), we identified decedents aged 15–84 years in whom infective endocarditis (ICD-10: I33.0, I33.9, I38) and cardiac device complications (ICD-10: T82.0, T82.2, T82.6, T82.7) were listed as contributing causes of death. Age-adjusted mortality rates (AAMRs) per 100,000 population were calculated using the 2000 U.S. standard population. Joinpoint regression (v5.4.0) identified inflection points in trends and calculated Annual Percent Change (APC).
Results:
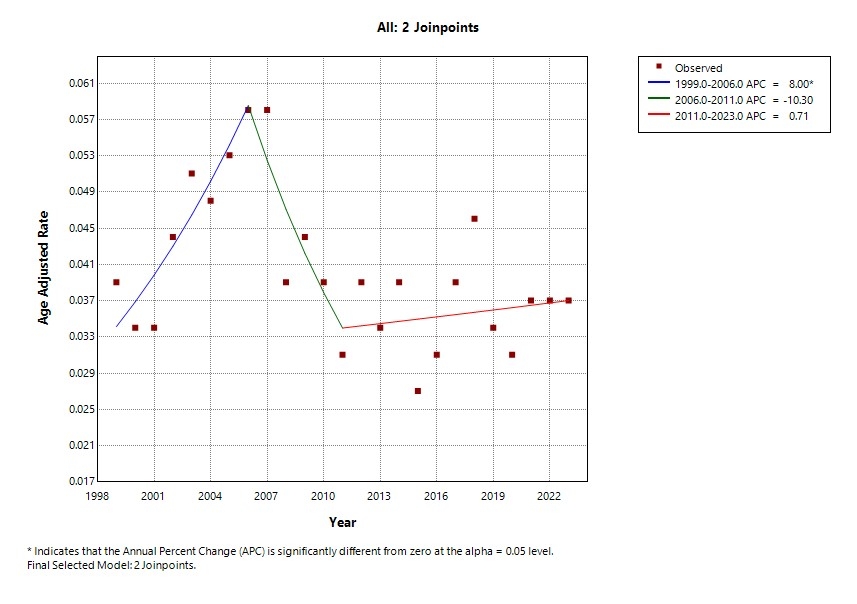
From 1999 to 2023, a final model with two joinpoints was identified. Between 1999 and 2006, AAMRs increased significantly with an APC of +8.00% (95% CI: 2.06 to 14.29; p = 0.01). This was followed by a sharp decline from 2006 to 2011 (APC = –10.30%; 95% CI: –20.90 to +1.72; p = 0.086). Between 2011 and 2023, mortality trends plateaued, with a modest but non-significant rise (APC = +0.71%; 95% CI: –1.57 to +3.06; p = 0.52). Overall, mortality rates stabilized over the last decade despite the earlier fluctuations.
Conclusion:
The trajectory of endocarditis-related mortality in patients with cardiac device complications reveals a critical inflection in modern cardiovascular care. The initial rise mirrors a surge in device utilization without parallel infection safeguards. The subsequent decline suggests early wins from antimicrobial stewardship and surgical protocol refinement. However, the post-2011 plateau, despite advances in materials and perioperative care, signals a stagnation point, not success. This stagnation likely reflects unresolved mechanistic challenges such as biofilm resilience, hematogenous microbial seeding, and late-onset device colonization. These findings position infective endocarditis as a high-fidelity surrogate for late device-related mortality burden. Urgent innovation is needed: biocompatible surface technologies, sustained post-implantation surveillance, and precision infection diagnostics must now lead the next phase of device-era infection prevention.
Cardiac devices such as prosthetic valves, coronary bypass grafts, and implantable hardware have improved survival but are associated with increased infection risk. Infective endocarditis (IE) remains a life-threatening complication of device-related infections. Despite advances in antimicrobial strategies and perioperative protocols, long-term national trends in endocarditis-related mortality with cardiac device complications remain under-characterized.
Methods:
Using the CDC WONDER Multiple Cause of Death database (1999–2023), we identified decedents aged 15–84 years in whom infective endocarditis (ICD-10: I33.0, I33.9, I38) and cardiac device complications (ICD-10: T82.0, T82.2, T82.6, T82.7) were listed as contributing causes of death. Age-adjusted mortality rates (AAMRs) per 100,000 population were calculated using the 2000 U.S. standard population. Joinpoint regression (v5.4.0) identified inflection points in trends and calculated Annual Percent Change (APC).
Results:
From 1999 to 2023, a final model with two joinpoints was identified. Between 1999 and 2006, AAMRs increased significantly with an APC of +8.00% (95% CI: 2.06 to 14.29; p = 0.01). This was followed by a sharp decline from 2006 to 2011 (APC = –10.30%; 95% CI: –20.90 to +1.72; p = 0.086). Between 2011 and 2023, mortality trends plateaued, with a modest but non-significant rise (APC = +0.71%; 95% CI: –1.57 to +3.06; p = 0.52). Overall, mortality rates stabilized over the last decade despite the earlier fluctuations.
Conclusion:
The trajectory of endocarditis-related mortality in patients with cardiac device complications reveals a critical inflection in modern cardiovascular care. The initial rise mirrors a surge in device utilization without parallel infection safeguards. The subsequent decline suggests early wins from antimicrobial stewardship and surgical protocol refinement. However, the post-2011 plateau, despite advances in materials and perioperative care, signals a stagnation point, not success. This stagnation likely reflects unresolved mechanistic challenges such as biofilm resilience, hematogenous microbial seeding, and late-onset device colonization. These findings position infective endocarditis as a high-fidelity surrogate for late device-related mortality burden. Urgent innovation is needed: biocompatible surface technologies, sustained post-implantation surveillance, and precision infection diagnostics must now lead the next phase of device-era infection prevention.
More abstracts on this topic:
Abatacept Drug-Induced Loeffler Endocarditis: A Manifestation of Hypereosinophilic Syndrome
Sweeting Alexander, Atalay Michael, Agarwal Saurabh, Hulten Edward, Patel Yash
Beyond Antibiotics: Transcatheter AngioVac Debulking of Right-Sided Methicillin-Resistant Staphylococcus aureus Endocarditis in a Hemodialysis PatientAghasili Chukwuemeka, Nawaz Haleema, Frimpong Smith, Hassan Rafla, Al-abboud Omar, Ahmad Tariq Ali