Final ID: MP271
Sex-Stratified Trends in Mortality from Cardiogenic Shock–Complicated Acute Myocardial Infarction: A 25-Year National Analysis Using CDC WONDER (1999–2023)
Abstract Body (Do not enter title and authors here): Background:
Cardiogenic shock (CS) remains the most lethal complication of acute myocardial infarction (AMI), with high mortality despite advances in revascularization and mechanical circulatory support. While sex-based differences in AMI presentation and outcomes are increasingly recognized, long-term trends in CS-complicated AMI mortality stratified by sex remain underexplored nationally. Understanding these trends is vital for addressing disparities and achieving equity in care.
Methods:
We analyzed 1999–2023 data from the CDC WONDER Multiple Cause of Death database, identifying U.S. decedents aged 15–84 with AMI (ICD-10: I21) as the underlying cause of death and CS (ICD-10: R57.0) as a contributing cause. Age-adjusted mortality rates (AAMRs) per 100,000 were calculated using the 2000 U.S. census standard and stratified by sex. Joinpoint regression (NCI v5.4.0) was used to detect inflection points and estimate Annual Percent Change (APC) and Average Annual Percent Change (AAPC) with 95% confidence intervals.
Results:
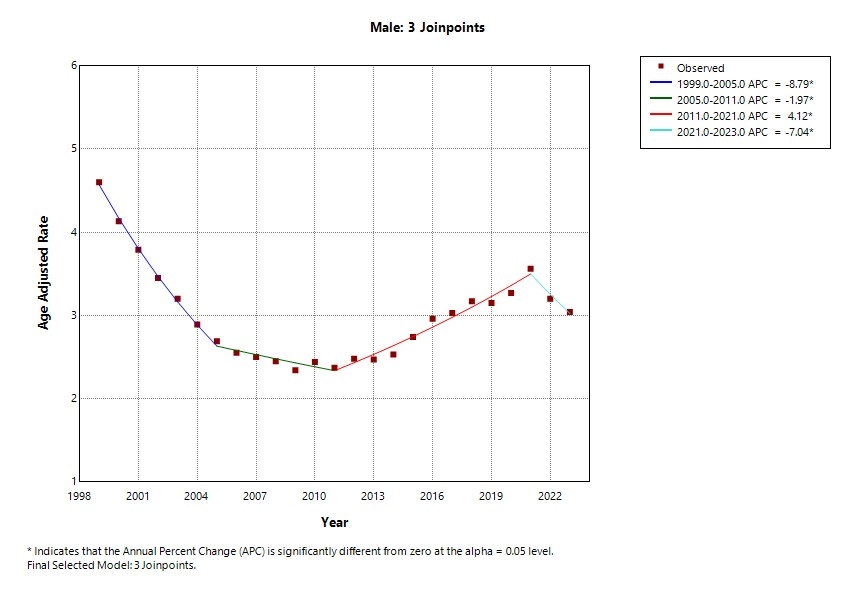
From 1999 to 2023, 90,207 male and 58,670 female deaths were identified. Male AAMRs declined from 4.60 to 3.04, with four phases: sharp decline (1999–2005, APC –8.79%, p<0.001), slower decline (2005–2011, –1.97%, p=0.03), sharp increase (2011–2021, +4.12%, p<0.001), and recent decline (2021–2023, –7.04%, p=0.017). Female AAMRs dropped from 2.76 to 1.52, with five phases: rapid decline (1999–2003, –10.42%, p<0.001), continued decline (2003–2009, –4.93%, p<0.001), plateau (2009–2013, +0.18%, p=0.92), sharp increase (2013–2021, +3.46%, p<0.001), and non-significant recent decline (2021–2023, –6.45%, p=0.058). While male mortality remained higher, a notable resurgence in female mortality rates occurred after 2013.
Conclusion:
Over 25 years, men consistently had higher mortality from CS-complicated AMI, yet a significant reversal in female trends after 2013 raises concern. This may reflect worsening risk profiles in older women, under-recognition of atypical symptoms, and lower use of invasive therapies such as PCI and mechanical support. The healthcare shift toward device-based care in the mid-2010s may have amplified sex-based disparities, given women's underrepresentation in trials. Modest recent improvements in female mortality suggest delayed progress. These findings call for sex-specific clinical pathways, equitable access to therapies, and stronger inclusion of women in CS research and planning to ensure just and effective cardiovascular care.
Cardiogenic shock (CS) remains the most lethal complication of acute myocardial infarction (AMI), with high mortality despite advances in revascularization and mechanical circulatory support. While sex-based differences in AMI presentation and outcomes are increasingly recognized, long-term trends in CS-complicated AMI mortality stratified by sex remain underexplored nationally. Understanding these trends is vital for addressing disparities and achieving equity in care.
Methods:
We analyzed 1999–2023 data from the CDC WONDER Multiple Cause of Death database, identifying U.S. decedents aged 15–84 with AMI (ICD-10: I21) as the underlying cause of death and CS (ICD-10: R57.0) as a contributing cause. Age-adjusted mortality rates (AAMRs) per 100,000 were calculated using the 2000 U.S. census standard and stratified by sex. Joinpoint regression (NCI v5.4.0) was used to detect inflection points and estimate Annual Percent Change (APC) and Average Annual Percent Change (AAPC) with 95% confidence intervals.
Results:
From 1999 to 2023, 90,207 male and 58,670 female deaths were identified. Male AAMRs declined from 4.60 to 3.04, with four phases: sharp decline (1999–2005, APC –8.79%, p<0.001), slower decline (2005–2011, –1.97%, p=0.03), sharp increase (2011–2021, +4.12%, p<0.001), and recent decline (2021–2023, –7.04%, p=0.017). Female AAMRs dropped from 2.76 to 1.52, with five phases: rapid decline (1999–2003, –10.42%, p<0.001), continued decline (2003–2009, –4.93%, p<0.001), plateau (2009–2013, +0.18%, p=0.92), sharp increase (2013–2021, +3.46%, p<0.001), and non-significant recent decline (2021–2023, –6.45%, p=0.058). While male mortality remained higher, a notable resurgence in female mortality rates occurred after 2013.
Conclusion:
Over 25 years, men consistently had higher mortality from CS-complicated AMI, yet a significant reversal in female trends after 2013 raises concern. This may reflect worsening risk profiles in older women, under-recognition of atypical symptoms, and lower use of invasive therapies such as PCI and mechanical support. The healthcare shift toward device-based care in the mid-2010s may have amplified sex-based disparities, given women's underrepresentation in trials. Modest recent improvements in female mortality suggest delayed progress. These findings call for sex-specific clinical pathways, equitable access to therapies, and stronger inclusion of women in CS research and planning to ensure just and effective cardiovascular care.
More abstracts on this topic:
A Case of Double Chambered Right Ventricle Associated with Ventricular Septal Defect- an Overlooked Congenital Heart Disease
Wang Roy, Gorantla Asher, Budzikowski Adam, Graham-hill Suzette, Bukharovich Inna, Abdulfattah Ammar, Palmer Wayne-andrew, Chandrakumar Harshith, Schaible Michael, Allison Elizabeth, Thambireddy Monica, Nnadi Ekenedilichukwu, Nevolina Anna
A Multicenter Friedreich Ataxia Registry Identifies Posterior Wall Thickness as a Predictor of Major Adverse Cardiac EventsLin Kimberly, Johnson Jonathan, Mccormack Shana, Lynch David, Tate Barbara, Feng Yixuan, Huang Jing, Mercer-rosa Laura, Dedio Anna, Mcsweeney Kara, Fournier Anne, Yoon Grace, Payne Ronald, Cripe Linda, Patel Aarti, Niaz Talha