Final ID: MP778
Prevalence and Post-Discharge Outcomes of Acute Noncardiac Organ Failure among Non-Acute Myocardial Infarction Cardiogenic Shock: A Nationwide Cohort Analysis
Abstract Body (Do not enter title and authors here): Introduction
Noncardiac organ failure is a frequent complication in non–acute myocardial infarction (non-AMI) cardiogenic shock (CS), which accounts for a substantial proportion of CS hospitalizations. Although overall outcomes in non-AMI CS have improved, the effect of noncardiac organ failure on post-discharge outcomes remains understudied.
Methods
Using the Nationwide Readmissions Database (2016–2021) we included non-AMI CS index hospitalizations among patients ≥ 18 years. Index hospitalizations were defined as patients discharged alive and prior to December of that year. After identifying acute kidney injury (AKI), acute neurological failure, acute hematologic failure, acute respiratory failure (ARF), and acute liver failure (ALF) during the index hospitalization, admissions were stratified into: no organ failure, single-system organ failure (OF), and multi-system OF (≥2 systems).
Primary outcomes were 30-day all-cause and heart failure (HF) readmission rates. Logistic regression was used to assess the association between OF and all-cause readmissions.
Results
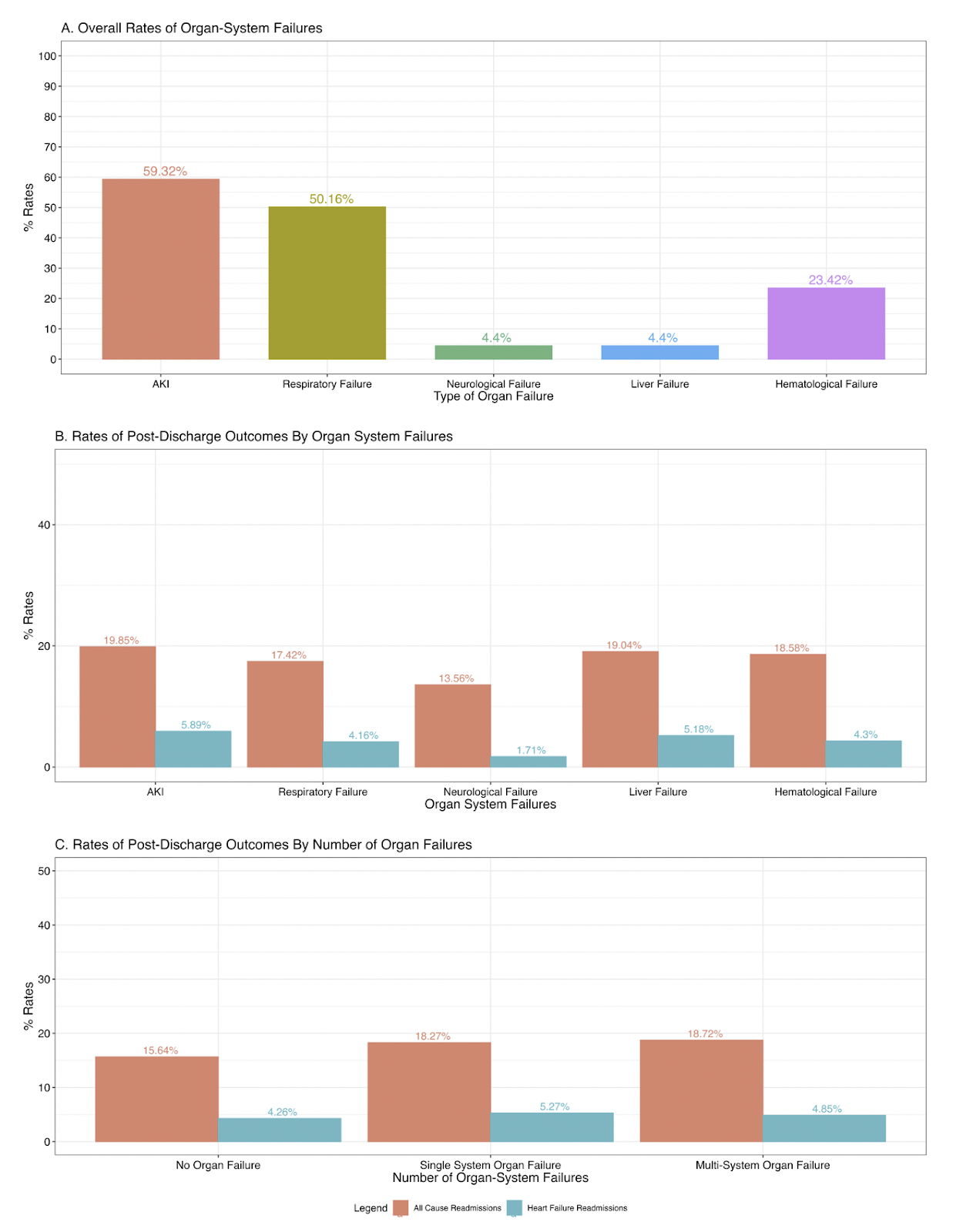
We identified 170,247 index non-AMI CS hospitalizations. The median age was 66 years (IQR 56–75); 63% were male, and 69% had chronic heart failure. AKI (59.96%) was the most common organ failure, followed by ARF (50.96%) (Fig 1A). In total, 48.22% developed multi-system OF, 35.96% had single-system OF, and 15.82% had no organ failure.
The overall 30-day all-cause and heart failure readmission rates were 18% and 4.9%, respectively. AKI was associated with the highest all-cause (19.85%) and HF (5.89%) readmission rates, followed by ALF (19.04% and 5.18%, respectively) (Fig 1B).
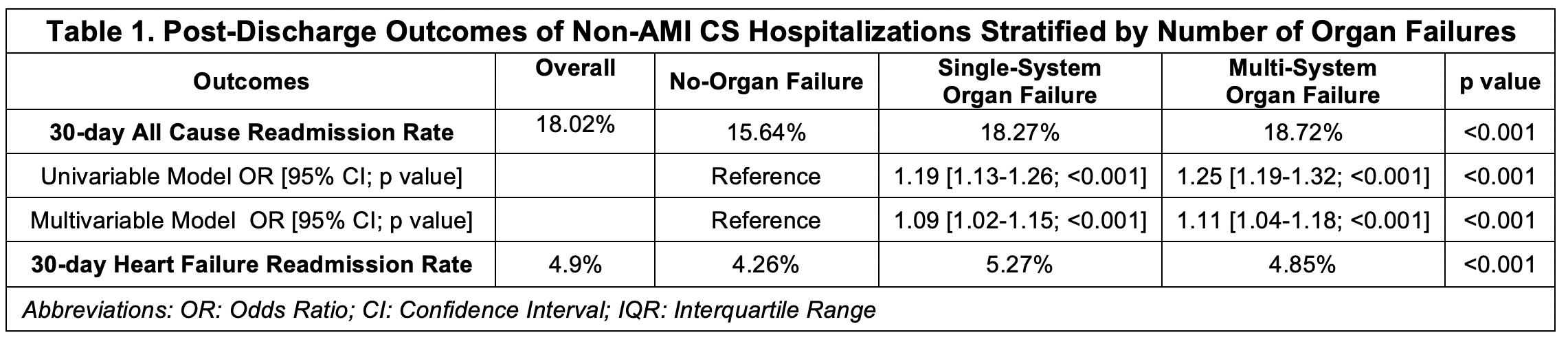
All-cause readmissions were highest in patients with multi-system OF (18.75%) compared to those with no organ failure (15.64%) (p < 0.001), while HF readmissions were highest in single-system OF (5.27%) (p < 0.001) (Fig 1C). After adjustment, both multi-system OF (aOR 1.11; 95% CI 1.04–1.18) and multi-system OF (aOR 1.09; 95% CI 1.02–1.15) were independently associated with increased odds of all-cause readmissions (Table 1).
Conclusion
Noncardiac organ failure during index non-AMI CS hospitalizations is linked to higher 30-day all-cause and HF readmission rates, with AKI showing the highest readmission rates. Both single and multi-system organ failure were independent predictors of all-cause readmissions, underscoring the importance of early post-discharge follow-up and multidisciplinary care planning for these high-risk patients.
Noncardiac organ failure is a frequent complication in non–acute myocardial infarction (non-AMI) cardiogenic shock (CS), which accounts for a substantial proportion of CS hospitalizations. Although overall outcomes in non-AMI CS have improved, the effect of noncardiac organ failure on post-discharge outcomes remains understudied.
Methods
Using the Nationwide Readmissions Database (2016–2021) we included non-AMI CS index hospitalizations among patients ≥ 18 years. Index hospitalizations were defined as patients discharged alive and prior to December of that year. After identifying acute kidney injury (AKI), acute neurological failure, acute hematologic failure, acute respiratory failure (ARF), and acute liver failure (ALF) during the index hospitalization, admissions were stratified into: no organ failure, single-system organ failure (OF), and multi-system OF (≥2 systems).
Primary outcomes were 30-day all-cause and heart failure (HF) readmission rates. Logistic regression was used to assess the association between OF and all-cause readmissions.
Results
We identified 170,247 index non-AMI CS hospitalizations. The median age was 66 years (IQR 56–75); 63% were male, and 69% had chronic heart failure. AKI (59.96%) was the most common organ failure, followed by ARF (50.96%) (Fig 1A). In total, 48.22% developed multi-system OF, 35.96% had single-system OF, and 15.82% had no organ failure.
The overall 30-day all-cause and heart failure readmission rates were 18% and 4.9%, respectively. AKI was associated with the highest all-cause (19.85%) and HF (5.89%) readmission rates, followed by ALF (19.04% and 5.18%, respectively) (Fig 1B).
All-cause readmissions were highest in patients with multi-system OF (18.75%) compared to those with no organ failure (15.64%) (p < 0.001), while HF readmissions were highest in single-system OF (5.27%) (p < 0.001) (Fig 1C). After adjustment, both multi-system OF (aOR 1.11; 95% CI 1.04–1.18) and multi-system OF (aOR 1.09; 95% CI 1.02–1.15) were independently associated with increased odds of all-cause readmissions (Table 1).
Conclusion
Noncardiac organ failure during index non-AMI CS hospitalizations is linked to higher 30-day all-cause and HF readmission rates, with AKI showing the highest readmission rates. Both single and multi-system organ failure were independent predictors of all-cause readmissions, underscoring the importance of early post-discharge follow-up and multidisciplinary care planning for these high-risk patients.
More abstracts on this topic:
A Case of Steroid-Refractory Immune-checkpoint-inhibitor Induced Myocarditis Responsive to Mycophenolate and Anti-thymocyte globulin
Dabdoub Jorge, Wilson Michael, Gottbrecht Matthew, Salazar Ryan, Shih Jeffrey
Ability of Composite Magnetic Resonance Brain Imaging Scores to Predict Functional Outcomes in Survivors of Cardiac ArrestNguyen Thuhien, Town James, Wahlster Sarah, Johnson Nicholas, Poilvert Nicolas, Lin Victor, Ukatu Hope, Matin Nassim, Davis Arielle, Taylor Breana, Thomas Penelope, Sharma Monisha