Final ID: Su3007
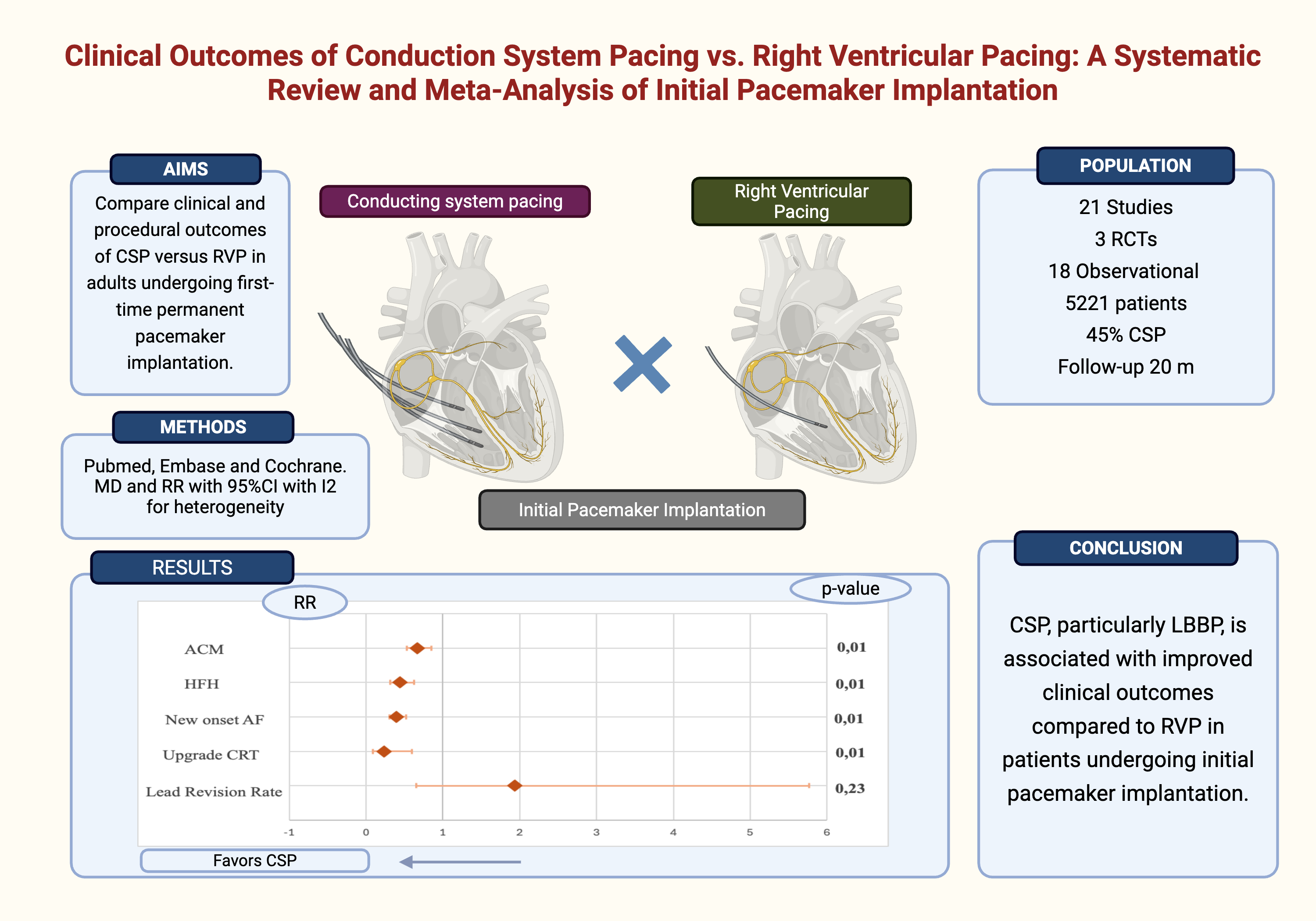
Clinical Outcomes of Conduction System Pacing Versus Right Ventricular Pacing: A Systematic Review and Meta-Analysis of Initial Pacemaker Implantation
Abstract Body (Do not enter title and authors here): Background: Right ventricular pacing (RVP) is the standard approach for bradyarrhythmia but is linked to adverse outcomes like pacing-induced cardiomyopathy and heart failure. Conduction system pacing (CSP), including His bundle pacing (HBP) and left bundle branch pacing (LBBP), offers a more physiologic alternative. However, its comparative effectiveness and safety versus RVP remain uncertain.
Research question: Does CSP improve clinical outcomes compared to RVP in patients receiving their first pacemaker?
Aims: To compare clinical and procedural outcomes of CSP versus RVP in adults undergoing first-time permanent pacemaker implantation.
Methods: We performed a systematic review and meta-analysis comparing CSP (HBP or LBBP) with RVP. Searches were conducted in PubMed, Embase, and Cochrane Library through April 2025. Outcomes included heart failure hospitalization (HFH), all-cause mortality, new-onset AF, upgrade to cardiac resynchronization therapy (CRT), left ventricular ejection fraction (LVEF) at follow-up, and lead revision rates. Random-effects models in R software (v4.4.1) were used to estimate risk ratios (RRs) or mean differences (MDs) with 95% confidence intervals (CIs). Subgroup analyses by pacing type (LBBP vs. HBP) were conducted.
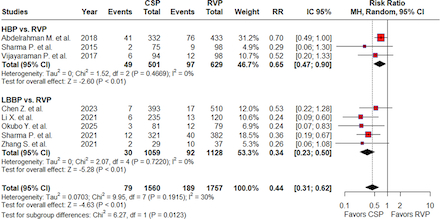
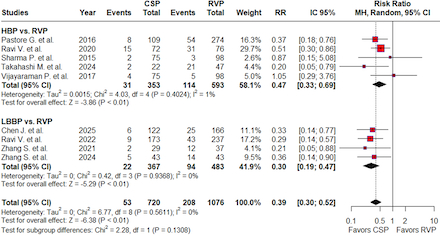
Results: Twenty-one studies (3 RCTs and 18 observational studies) comprising 5,232 patients were included, of whom 2,360 (45%) underwent CSP. Seven studies evaluated HBP (1,822 patients), and 14 evaluated LBBP (3,399 patients). The mean follow-up was 20 months. CSP was associated with significantly lower risks of HFH (RR 0.44; 95% CI 0.31–0.62; p < 0.01; Figure 2), new-onset AF (RR 0.39; 95% CI 0.30–0.52; p<0.01; Figure 3), all-cause mortality (RR 0.67; 95% CI 0.53–0.85; p=0.01), and upgrade to CRT (RR 0.23; 95% CI 0.09–0.60; p<0.01). LVEF was significantly higher in the CSP group (MD 2.13%; 95% CI 0.48–3.79; p=0.01). No significant difference was observed in lead revision rates (RR 1.94; 95% CI 0.65–5.77; p=0.23). Subgroup analyses showed the superiority of LBBP over HBP for all outcomes (pinteraction<0.01), except for new-onset AF and LVEF improvement (pinteraction>0.05). HBP was associated with a higher lead revision rate than LBBP (pinteraction<0.01).
Conclusion: CSP, particularly LBBP, is associated with improved clinical outcomes compared to RVP in patients undergoing initial pacemaker implantation. These findings support CSP as a more physiologic pacing strategy with a favorable safety and efficacy profile.
Research question: Does CSP improve clinical outcomes compared to RVP in patients receiving their first pacemaker?
Aims: To compare clinical and procedural outcomes of CSP versus RVP in adults undergoing first-time permanent pacemaker implantation.
Methods: We performed a systematic review and meta-analysis comparing CSP (HBP or LBBP) with RVP. Searches were conducted in PubMed, Embase, and Cochrane Library through April 2025. Outcomes included heart failure hospitalization (HFH), all-cause mortality, new-onset AF, upgrade to cardiac resynchronization therapy (CRT), left ventricular ejection fraction (LVEF) at follow-up, and lead revision rates. Random-effects models in R software (v4.4.1) were used to estimate risk ratios (RRs) or mean differences (MDs) with 95% confidence intervals (CIs). Subgroup analyses by pacing type (LBBP vs. HBP) were conducted.
Results: Twenty-one studies (3 RCTs and 18 observational studies) comprising 5,232 patients were included, of whom 2,360 (45%) underwent CSP. Seven studies evaluated HBP (1,822 patients), and 14 evaluated LBBP (3,399 patients). The mean follow-up was 20 months. CSP was associated with significantly lower risks of HFH (RR 0.44; 95% CI 0.31–0.62; p < 0.01; Figure 2), new-onset AF (RR 0.39; 95% CI 0.30–0.52; p<0.01; Figure 3), all-cause mortality (RR 0.67; 95% CI 0.53–0.85; p=0.01), and upgrade to CRT (RR 0.23; 95% CI 0.09–0.60; p<0.01). LVEF was significantly higher in the CSP group (MD 2.13%; 95% CI 0.48–3.79; p=0.01). No significant difference was observed in lead revision rates (RR 1.94; 95% CI 0.65–5.77; p=0.23). Subgroup analyses showed the superiority of LBBP over HBP for all outcomes (pinteraction<0.01), except for new-onset AF and LVEF improvement (pinteraction>0.05). HBP was associated with a higher lead revision rate than LBBP (pinteraction<0.01).
Conclusion: CSP, particularly LBBP, is associated with improved clinical outcomes compared to RVP in patients undergoing initial pacemaker implantation. These findings support CSP as a more physiologic pacing strategy with a favorable safety and efficacy profile.
More abstracts on this topic:
Durability of Left Bundle Branch Area Capture over Time: A Single Center Retrospective Analysis
Jafry Ali, Cherian Tharian, Noory Ali, Thosani Amit, Silverstein Joshua, Liu Emerson, Belden William, Chenarides John, Friehling Mati, Shaw George
Aortic Tortuosity Predicts Conduction Disturbances After TAVR via Aortic Angle and Membranous Septum Length: A Structural Equation Modeling ApproachNakamura Takamitsu, Horikoshi Takeo, Eguchi Miu, Kobayashi Tsuyoshi, Uematsu Manabu, Yoshizaki Toru, Sato Akira