Final ID: MP1289
Multi-parametric Cardiac MRI predicts cardiovascular outcomes in HTx recipients after long-term follow-up
Abstract Body (Do not enter title and authors here): Background:
The long-term survival of heart transplantation (HTx) recipients is influenced by a range of cardiovascular, immunological, and procedural factors. Accurately predicting post-HTx outcomes remains a major clinical challenge, especially when relying solely on noninvasive methods.
Objective:
To test the hypothesis that structural and functional indices derived from multi-parametric cardiac MRI-derived can be used to predict cardiovascular events in HTx recipients.
Materials and methods:
With the approval of institutional review board (IRB), 170 HTx recipients (106 males, age: 47.8 ± 16 years, Range: 19 – 79 years) were recruited for a comprehensive multi-parametric cardiac MRI scan. MRI images were processed to derive global cardiac function and volumes, and myocardial T2 values and T1 values. Pre- and post-Gadolinium T1 was used to calculate extra-cellular volume (ECV) fraction. Cardiovascular events were defined as a composite of any emergency visit, hospitalization or death due to graft failure or reception, myocardial infarction, HF and other events that cannot rule out a cardiovascular origin of complications. Identification of predictors of adverse outcomes at long-term follow-up was based on a Cox proportional hazards model (CPH). Statistical analysis was performed by using SPSS (version 22.0).
Results:
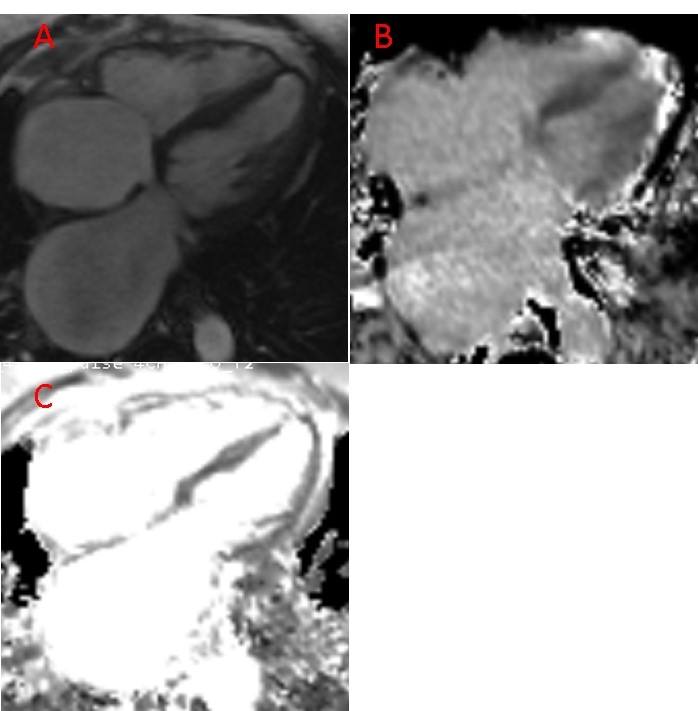
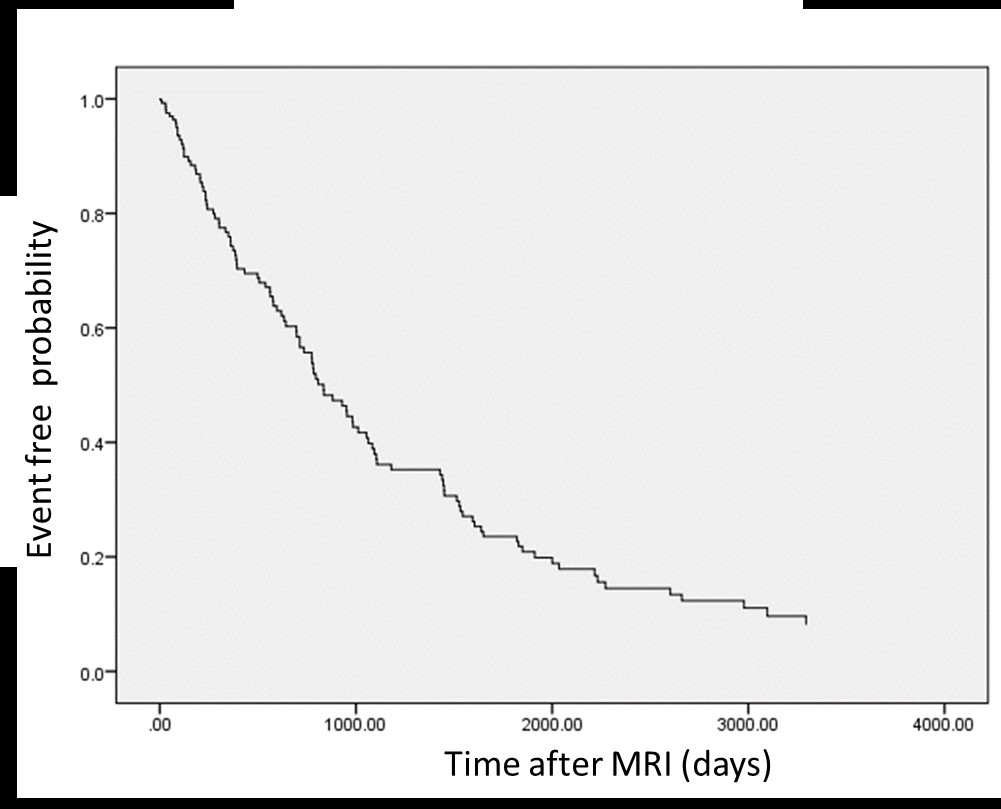
MRI images were eligilbe for quantitative analysis. See figure 1. The patients were followed for 6 to 4504 days (Median = 2616 days) after multi-parametric cardiac MRI. In total, 140 cardiovascular events occurred (6 to 3294 days, Median = 627 days). The CPH model fits the data (p < 0.001). After the adjustment of traditional cardiovascular risk factors and demographic data, multiple MRI-derived indices were identified as significant predictors of survival time (time between baseline cardiac MRI and adverse event), including left ventricular (LV) end-diastolic volume (LVEDV) (p < 0.001), LV end-systolic volume (LVESV) (p < 0.001), LV stroke volume (LVSV) (p = 0.005), right ventricular (RV) stroke volume (RVSV) (p < 0.001), RV cardiac output (RVCO) ( p = 0.03), myocardial ECV (p < 0.001) and T2 value (p = 0.008). See figure 2.
Conclusions:
Multi-parametric indices of cardiac tissue (T2, ECV) and function (LVEDV, LVESV, LVSV, RVSV, RVCO) can independently predict adverse clinical outcomes in HTx recipients at long term follow-up (median > 7 years). MRI may offer new imaging biomarkers for early identification of risks for post-HTx complication.
The long-term survival of heart transplantation (HTx) recipients is influenced by a range of cardiovascular, immunological, and procedural factors. Accurately predicting post-HTx outcomes remains a major clinical challenge, especially when relying solely on noninvasive methods.
Objective:
To test the hypothesis that structural and functional indices derived from multi-parametric cardiac MRI-derived can be used to predict cardiovascular events in HTx recipients.
Materials and methods:
With the approval of institutional review board (IRB), 170 HTx recipients (106 males, age: 47.8 ± 16 years, Range: 19 – 79 years) were recruited for a comprehensive multi-parametric cardiac MRI scan. MRI images were processed to derive global cardiac function and volumes, and myocardial T2 values and T1 values. Pre- and post-Gadolinium T1 was used to calculate extra-cellular volume (ECV) fraction. Cardiovascular events were defined as a composite of any emergency visit, hospitalization or death due to graft failure or reception, myocardial infarction, HF and other events that cannot rule out a cardiovascular origin of complications. Identification of predictors of adverse outcomes at long-term follow-up was based on a Cox proportional hazards model (CPH). Statistical analysis was performed by using SPSS (version 22.0).
Results:
MRI images were eligilbe for quantitative analysis. See figure 1. The patients were followed for 6 to 4504 days (Median = 2616 days) after multi-parametric cardiac MRI. In total, 140 cardiovascular events occurred (6 to 3294 days, Median = 627 days). The CPH model fits the data (p < 0.001). After the adjustment of traditional cardiovascular risk factors and demographic data, multiple MRI-derived indices were identified as significant predictors of survival time (time between baseline cardiac MRI and adverse event), including left ventricular (LV) end-diastolic volume (LVEDV) (p < 0.001), LV end-systolic volume (LVESV) (p < 0.001), LV stroke volume (LVSV) (p = 0.005), right ventricular (RV) stroke volume (RVSV) (p < 0.001), RV cardiac output (RVCO) ( p = 0.03), myocardial ECV (p < 0.001) and T2 value (p = 0.008). See figure 2.
Conclusions:
Multi-parametric indices of cardiac tissue (T2, ECV) and function (LVEDV, LVESV, LVSV, RVSV, RVCO) can independently predict adverse clinical outcomes in HTx recipients at long term follow-up (median > 7 years). MRI may offer new imaging biomarkers for early identification of risks for post-HTx complication.
More abstracts on this topic:
A Trial of Patients Receiving Remote Ischemic Conditioning in Early Stroke (PRICES) in a Tertiary Hospital in the Philippines: An Open Label Study
Ang Kevin Royce, Juangco Dan, Hernandez Maria Kim
Acoramidis Effect on All-Cause Mortality in Patients with p.V142I (V122I) Variant ATTR-CM: Findings From the ATTRibute-CM StudyAlexander Kevin, Bhatt Kunal, Judge Daniel, Grodin Justin, Akinboboye Olakunle, Chen Chris, Tamby Jean-francois, Castano Adam, Fox Jonathan, Fontana Marianna, Gillmore Julian, Sarswat Nitasha, Grogan Martha, Solomon Scott, Davis Margot, Cuddy Sarah, Kittleson Michelle, Shah Keyur, Griffin Jan, Ruberg Frederick, Khouri Michel