Final ID: Su4157
Patients with Atrial Fibrillation who Maintain Sinus Rhythm post Ablation Demonstrate Improved Left Atrial Blood Flow and Volume
Abstract Body (Do not enter title and authors here): Introduction: Atrial Fibrillation (AF) incidence increased by 30% over the past 20 years with 1 of 7 strokes attributed to AF. While catheter ablation (CA) is valuable at decreasing AF burden, its long-term effect on stroke risk is unknown. 4D flow MRI studies of AF patients have found reduced peak velocities and increased blood stasis in the left atrium (LA) and LA appendage (LAA), indicating AF-associated atrial flow impairment and increased thromboembolism risk.
Aim: To explore, using 4D flow MRI, pre vs post-CA LA and LAA hemodynamics and volumes in patients with and without AF recurrence.
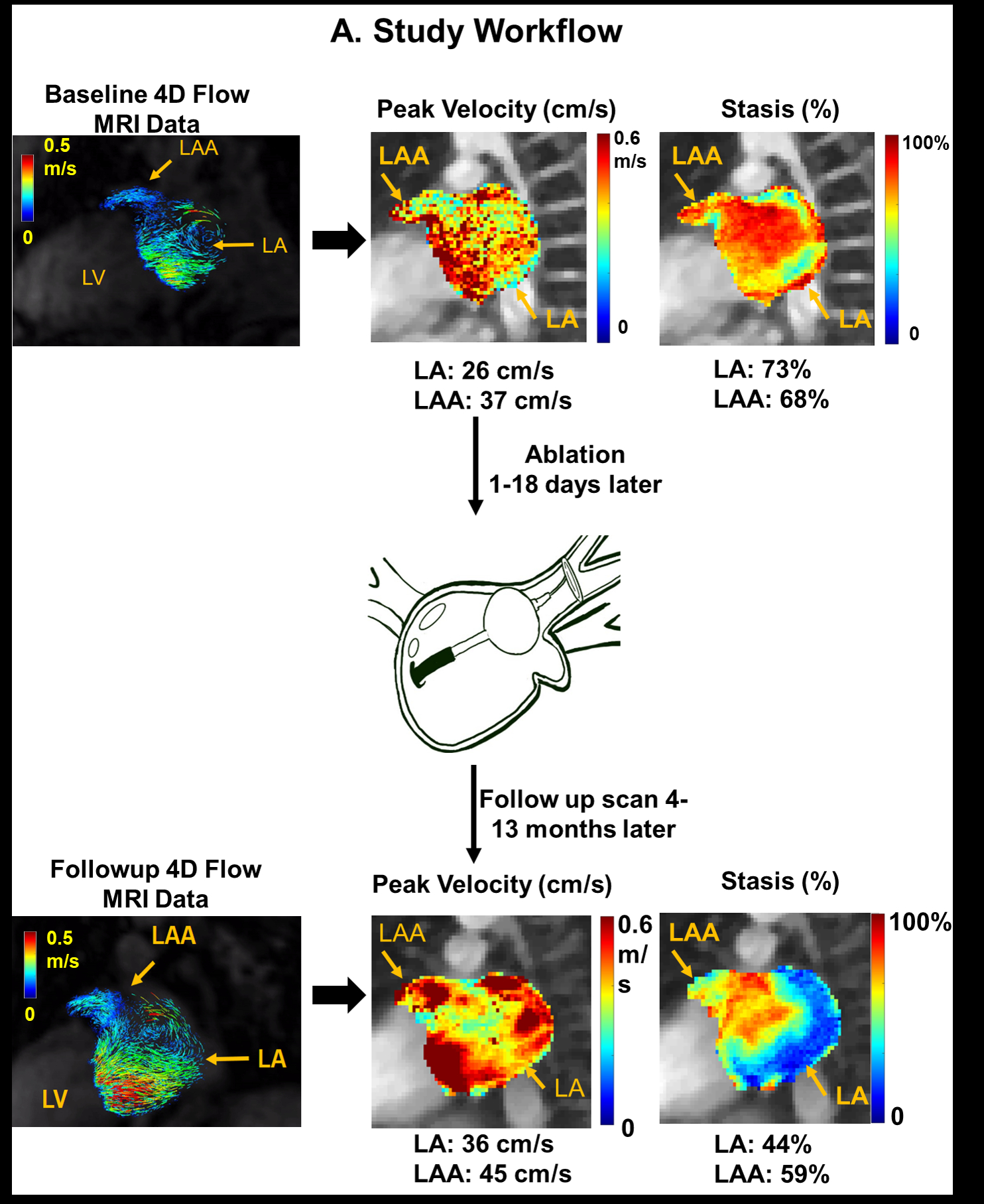
Methods: We enrolled 60 AF patients who had baseline (pre-CA) and follow-up (post-CA) 4D-flow MRI scans. Success was defined as no recurrent AF > 30 sec on intermittent monitoring after a 3-month blanking period. 4D flow data analysis included pre-processing and LA/LAA manual 3D segmentation. The segmentations were used to calculate LA and LAA volumes as well as peak velocity and blood stasis (Figure 1).
Results: Of the 60 patients (61.1 ± 12.3 years, 73% male), forty-five maintained SR while 15 had AF recurrence post-CA. One LAA was excluded from the analysis due to the presence of an artifact.
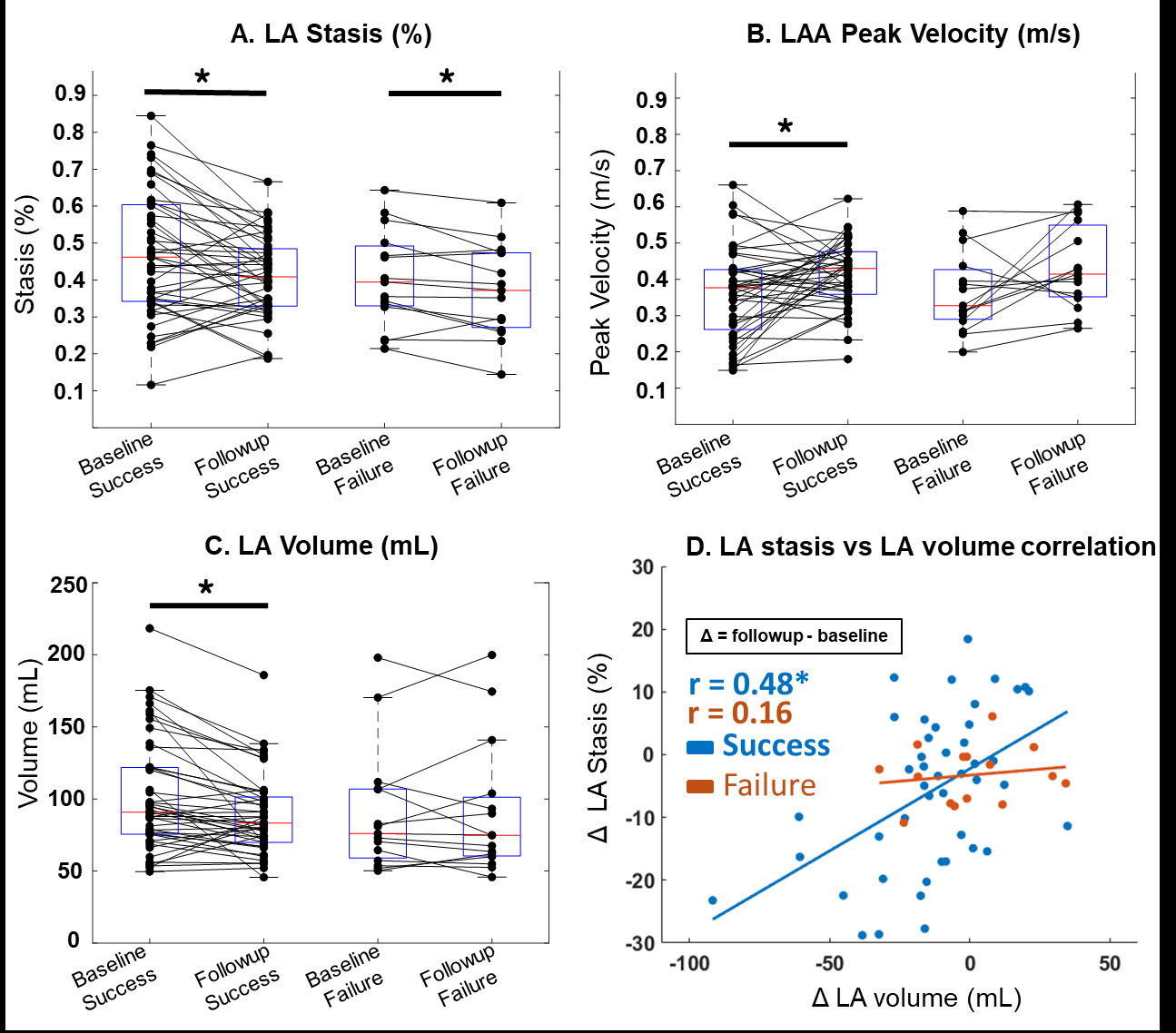
Mean LA stasis significantly decreased for both groups post-CA (success: 46 ± 17% to 41 ± 11% and failure: 40 ± 13% to 37 ± 12%, p <0.05). However, only the success group’s LAA peak velocity (36 ± 0.15 cm/s to 41.5 ± 0.09 cm/s, p <0.05) and LA volume (101 ± 39 ml to 89 ± 28 ml, p <0.05) changed significantly (Figure 2 A-C). Further, the change in LA stasis was strongly correlated (r=0.48, p <0.01) with the change in LA volume only in the success group (Figure 2D).
Conclusions: Our results reinforce that SR maintenance post-CA is key for improved LA flow and geometry, indicating that reverse remodeling is taking place. The LAA velocity change in those with successful CA may confer reduced thrombotic risk, since thrombus formation is linked to a reduced LAA velocity.
Aim: To explore, using 4D flow MRI, pre vs post-CA LA and LAA hemodynamics and volumes in patients with and without AF recurrence.
Methods: We enrolled 60 AF patients who had baseline (pre-CA) and follow-up (post-CA) 4D-flow MRI scans. Success was defined as no recurrent AF > 30 sec on intermittent monitoring after a 3-month blanking period. 4D flow data analysis included pre-processing and LA/LAA manual 3D segmentation. The segmentations were used to calculate LA and LAA volumes as well as peak velocity and blood stasis (Figure 1).
Results: Of the 60 patients (61.1 ± 12.3 years, 73% male), forty-five maintained SR while 15 had AF recurrence post-CA. One LAA was excluded from the analysis due to the presence of an artifact.
Mean LA stasis significantly decreased for both groups post-CA (success: 46 ± 17% to 41 ± 11% and failure: 40 ± 13% to 37 ± 12%, p <0.05). However, only the success group’s LAA peak velocity (36 ± 0.15 cm/s to 41.5 ± 0.09 cm/s, p <0.05) and LA volume (101 ± 39 ml to 89 ± 28 ml, p <0.05) changed significantly (Figure 2 A-C). Further, the change in LA stasis was strongly correlated (r=0.48, p <0.01) with the change in LA volume only in the success group (Figure 2D).
Conclusions: Our results reinforce that SR maintenance post-CA is key for improved LA flow and geometry, indicating that reverse remodeling is taking place. The LAA velocity change in those with successful CA may confer reduced thrombotic risk, since thrombus formation is linked to a reduced LAA velocity.
More abstracts on this topic:
A combined approach of cardiac magnetic resonance and CardioMEMS to assess right ventricular dysfunction during exercise in HFpEF-PH
Bekhuis Youri, Bogaert Jan, La Gerche Andre, Claessen Guido, Janssens Stefan, Droogne Walter, Rosseel Thomas, Barrios Leticia, Verwerft Jan, Timmermans Philippe, Trenson Sander, Dresselaers Tom
12,13-diHOME Attenuates Pro-Arrhythmic Effect of High-Fat DietBuck Benjamin, Baer Lisa, Deschenes Isabelle, Chinthalapudi Krishna, Gallego-perez Daniel, Stanford Kristin, Hund Thomas, Areiza Natalia, Xu Xianyao, Elliott Austin, Wan Xiaoping, Nassal Drew, Lane Cemantha, Nirengi Shinsuke, James Natasha Maria