Final ID: Sa1002
Cardiopulmonary Bypass and Aortic Cross-Clamp Times as Predictors of Outcomes in ECMO-Supported Cardiotomy Patients
Abstract Body (Do not enter title and authors here): Introduction:
Cardiopulmonary bypass time (CPBT) and aortic cross-clamp time (AXCT) are independently associated with postoperative morbidity and mortality. However, no universally accepted “optimal” duration exists, as these times are influenced by the complexity of cardiac surgery. ECMO is being increasingly used for cardiogenic shock in patients undergoing cardiotomy, but the impact of CPBT and AXCT on outcomes in this specific population remains unexplored. This study investigates how CPBT and AXCT influence outcomes in cardiotomy patients on ECMO support.
Research Question:
Do CPBT and AXCT influence mortality and complication rates in cardiotomy patients receiving ECMO support?
Methods:
We conducted a retrospective chart review (Jan 2020–Dec 2024) across a multidisciplinary North American practice, identifying 623 patients who required ECMO. Of these, 236 (37.8%) received ECMO in the preoperative, intraoperative, or postoperative period of cardiotomy. Patients were grouped by prolonged CPBT (>150 min) vs standard (≤150 min) and prolonged AXCT (>90 min) vs standard (≤90 min). We analyzed outcomes including 30-day mortality, ECMO characteristics, and postoperative complications.
Results:
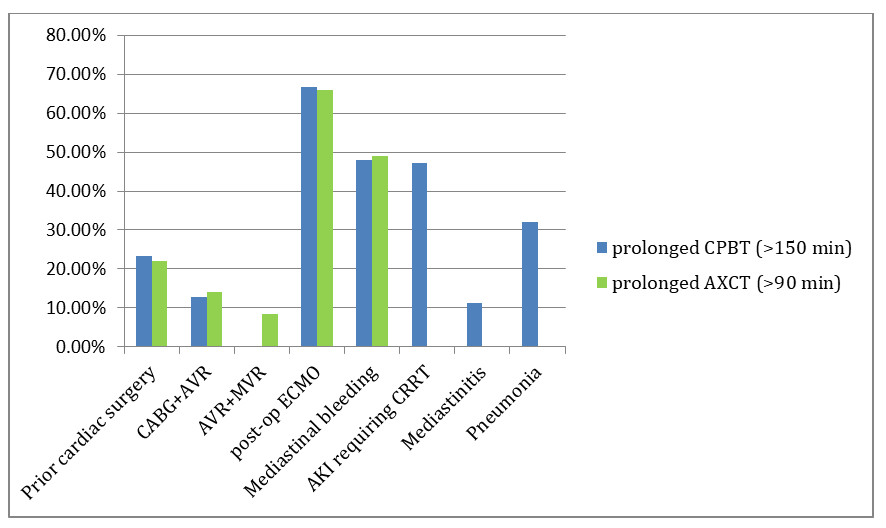
Among the 236 patients, the average age was 60.8 years, BMI 37.43 kg/m2; 63% were male, 85% White. Prolonged CPBT and AXCT were associated with higher BMI (p=0.02, 0.03), prior cardiac surgery (p<0.001, 0.006), and combined CABG+AVR procedures (p=0.01, 0.001). Patients with prolonged durations were more likely to require postoperative ECMO (p=0.001, 0.03). Complications such as mediastinal bleeding, AKI requiring CRRT, mediastinitis, bacteremia, and pneumonia, showed significant association with increased CPBT whereas prolonged AXCT was only linked with mediastinal bleeding. CPBT and AXCT durations did not significantly affect 30-day mortality, ICU/hospital stay, ECMO duration, or ventilation duration. Independent predictors of 30-day mortality included pre-/intraoperative IABP use (OR 2.19, 95% CI 1.11–4.30, p=0.023), Impella use (OR 0.20, 95% CI 0.03–0.75, p=0.040), post-op intracranial bleeding (OR 5.46, 95% CI 1.43–23.9, p=0.016), and CRRT-requiring AKI (OR 3.24, 95% CI 1.63–6.57, p<0.001).
Conclusion:
Prolonged CPBT and AXCT were significantly linked to higher rates of postoperative complications such as mediastinal bleeding, CRRT requiring AKI, mediastinitis, and pneumonia along with increased need for postoperative ECMO support, without significantly affecting mortality.
Cardiopulmonary bypass time (CPBT) and aortic cross-clamp time (AXCT) are independently associated with postoperative morbidity and mortality. However, no universally accepted “optimal” duration exists, as these times are influenced by the complexity of cardiac surgery. ECMO is being increasingly used for cardiogenic shock in patients undergoing cardiotomy, but the impact of CPBT and AXCT on outcomes in this specific population remains unexplored. This study investigates how CPBT and AXCT influence outcomes in cardiotomy patients on ECMO support.
Research Question:
Do CPBT and AXCT influence mortality and complication rates in cardiotomy patients receiving ECMO support?
Methods:
We conducted a retrospective chart review (Jan 2020–Dec 2024) across a multidisciplinary North American practice, identifying 623 patients who required ECMO. Of these, 236 (37.8%) received ECMO in the preoperative, intraoperative, or postoperative period of cardiotomy. Patients were grouped by prolonged CPBT (>150 min) vs standard (≤150 min) and prolonged AXCT (>90 min) vs standard (≤90 min). We analyzed outcomes including 30-day mortality, ECMO characteristics, and postoperative complications.
Results:
Among the 236 patients, the average age was 60.8 years, BMI 37.43 kg/m2; 63% were male, 85% White. Prolonged CPBT and AXCT were associated with higher BMI (p=0.02, 0.03), prior cardiac surgery (p<0.001, 0.006), and combined CABG+AVR procedures (p=0.01, 0.001). Patients with prolonged durations were more likely to require postoperative ECMO (p=0.001, 0.03). Complications such as mediastinal bleeding, AKI requiring CRRT, mediastinitis, bacteremia, and pneumonia, showed significant association with increased CPBT whereas prolonged AXCT was only linked with mediastinal bleeding. CPBT and AXCT durations did not significantly affect 30-day mortality, ICU/hospital stay, ECMO duration, or ventilation duration. Independent predictors of 30-day mortality included pre-/intraoperative IABP use (OR 2.19, 95% CI 1.11–4.30, p=0.023), Impella use (OR 0.20, 95% CI 0.03–0.75, p=0.040), post-op intracranial bleeding (OR 5.46, 95% CI 1.43–23.9, p=0.016), and CRRT-requiring AKI (OR 3.24, 95% CI 1.63–6.57, p<0.001).
Conclusion:
Prolonged CPBT and AXCT were significantly linked to higher rates of postoperative complications such as mediastinal bleeding, CRRT requiring AKI, mediastinitis, and pneumonia along with increased need for postoperative ECMO support, without significantly affecting mortality.
More abstracts on this topic:
Breaking New Ground in Prehospital Medicine: The Impact of Prehospital ECPR in Japan - A 14-Patient Case Study
Fujita Kensuke, Hagiwara Yoshihiro, Ogura Takayuki
Comparative Outcomes of Intra-Aortic Balloon Pump Versus Impella in Non-Myocardial Infarction Cardiogenic Shock: A National Inpatient Sample Database AnalysisKhalil Omar, White Amirah, Liu Qi, Kontos Michael, Shah Keyur, Li Pengyang, Saed Aldien Arwa, Patel Aditi, Cai Peng, Krayem Hussein, Ghoussaini Racha, Roberts Charlotte, Rao Krishnasree, Cooke Richard