Final ID: Sa2127
A rare case of ventriculobronchial fistula caused by an epicardial defibrillator patch
Abstract Body (Do not enter title and authors here): Background
Epicardial patch defibrillators (EPDs) were commonly implanted in the 1990s for secondary prevention of sudden cardiac death. Despite being largely obsolete, some EPDs remain in patients and can cause late complications. This case highlights such a scenario.
Case
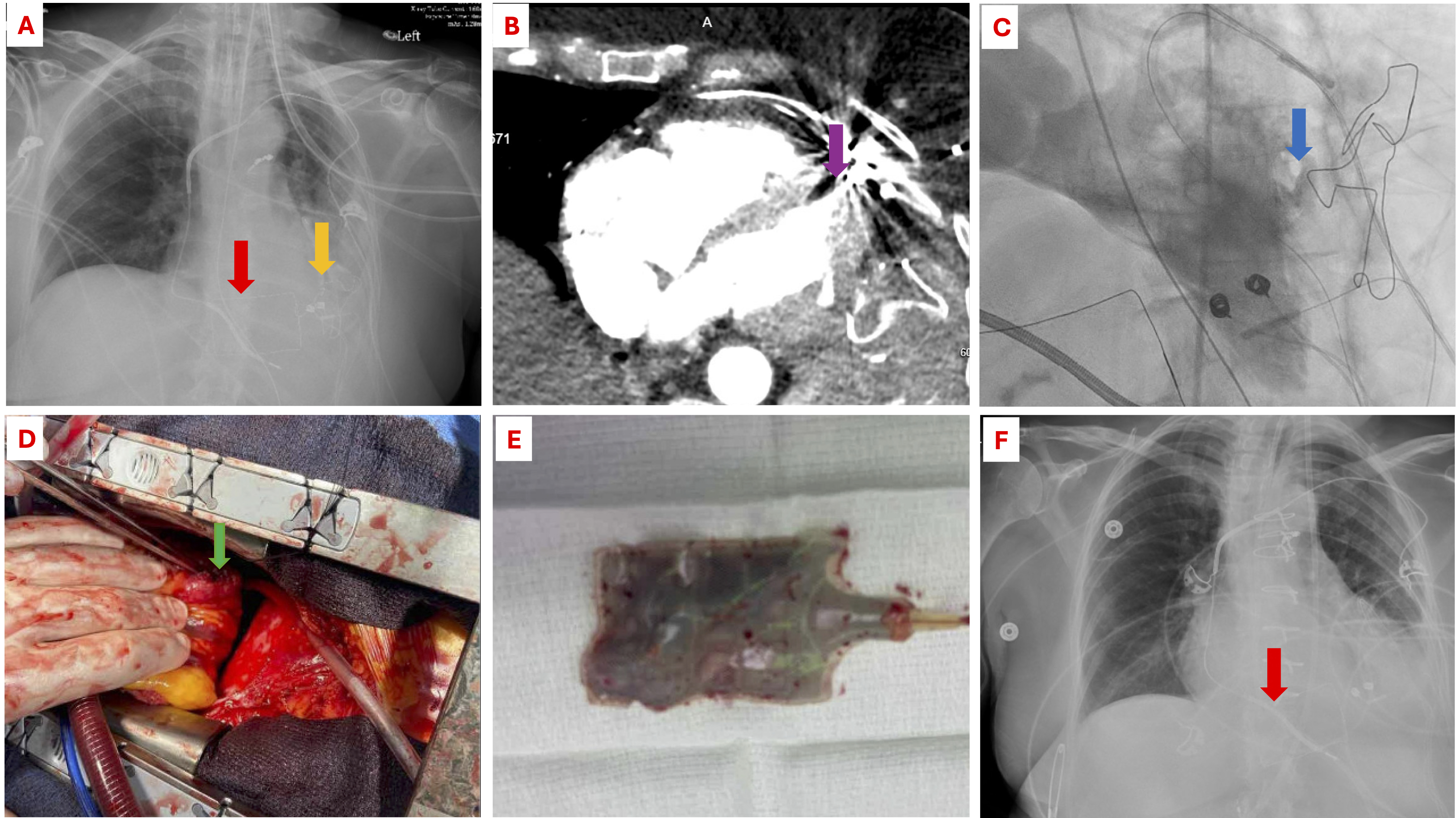
A 75-year-old female with a history of cardiac arrest 30 years ago presented with shortness of breath and left leg swelling. She had idiopathic ventricular fibrillation in 1992, treated with an EPD (Picture 1A), later replaced by a transvenous ICD.
She was diagnosed with left femoral deep venous thrombosis and bilateral pulmonary embolism and started on therapeutic anticoagulation. She experienced massive hemoptysis, leading to respiratory and cardiac arrest, but was resuscitated. A CT angiogram showed no active bleeding but noted the EPD was close to the lower lobe of the left lung. Upper gastrointestinal endoscopy showed no active bleeding. Bronchoscopy revealed clots in the left lower lobe. Despite empiric bronchial artery embolization, hemoptysis persisted. A repeat bronchoscopy showed reaccumulation of clots. A repeat CT angiogram indicated contrast extension into the ventricular myocardium near the EPD but no lung spillage suggestive of pseudoaneurysm (Picture 1B).
She was transferred to our institution for further evaluation. A coronary angiogram revealed normal arteries, while a left ventriculogram revealed contrast extravasation through the lateral wall (Picture 1C). An urgent surgery revealed two EPDs: anterior and lateral. The lateral EPD had eroded into the ventricle, creating a ventriculo bronchial fistula (Picture 1D). The lateral EPD was removed (Picture 1E); the anterior EPD was left in place (Picture 1F). The ventricular defect was debrided and repaired. Postoperative recovery was successful, with no further hemoptysis, and the patient was discharged to a rehabilitation facility.
Discussion
EPDs are no longer used due to high failure rates and complications like scar formation and constrictive pericarditis. However, patients with EPDs from the 1990s may present with delayed complications. Accurate diagnosis using multimodality imaging and early management is crucial to reduce morbidity and mortality.
Epicardial patch defibrillators (EPDs) were commonly implanted in the 1990s for secondary prevention of sudden cardiac death. Despite being largely obsolete, some EPDs remain in patients and can cause late complications. This case highlights such a scenario.
Case
A 75-year-old female with a history of cardiac arrest 30 years ago presented with shortness of breath and left leg swelling. She had idiopathic ventricular fibrillation in 1992, treated with an EPD (Picture 1A), later replaced by a transvenous ICD.
She was diagnosed with left femoral deep venous thrombosis and bilateral pulmonary embolism and started on therapeutic anticoagulation. She experienced massive hemoptysis, leading to respiratory and cardiac arrest, but was resuscitated. A CT angiogram showed no active bleeding but noted the EPD was close to the lower lobe of the left lung. Upper gastrointestinal endoscopy showed no active bleeding. Bronchoscopy revealed clots in the left lower lobe. Despite empiric bronchial artery embolization, hemoptysis persisted. A repeat bronchoscopy showed reaccumulation of clots. A repeat CT angiogram indicated contrast extension into the ventricular myocardium near the EPD but no lung spillage suggestive of pseudoaneurysm (Picture 1B).
She was transferred to our institution for further evaluation. A coronary angiogram revealed normal arteries, while a left ventriculogram revealed contrast extravasation through the lateral wall (Picture 1C). An urgent surgery revealed two EPDs: anterior and lateral. The lateral EPD had eroded into the ventricle, creating a ventriculo bronchial fistula (Picture 1D). The lateral EPD was removed (Picture 1E); the anterior EPD was left in place (Picture 1F). The ventricular defect was debrided and repaired. Postoperative recovery was successful, with no further hemoptysis, and the patient was discharged to a rehabilitation facility.
Discussion
EPDs are no longer used due to high failure rates and complications like scar formation and constrictive pericarditis. However, patients with EPDs from the 1990s may present with delayed complications. Accurate diagnosis using multimodality imaging and early management is crucial to reduce morbidity and mortality.
More abstracts on this topic:
Catheter Ablation for Ventricular Tachycardia in Ischemic Cardiomyopathy: A Meta-Analysis with Reconstructed Time-to-Event and Trial Sequential Analysis
Elbenawi Hossam, Kalaiger Abdul Mukhtadir, Ibrahim Ahmed, Eisa Mahmoud, Ibrahim Ramzi, Zaaya Morad, Tan Min Choon, Almaadawy Omar, Quelal Analuisa Karol, Ul Abideen Asad Zain, Lee Justin, Elsalmouny Youmna, Siontis Konstantinos, Del-carpio Munoz Freddy, Desimone Christopher, Deshmukh Abhishek, Mohamed Kareem, Hashim Ahmed, Agarwal Siddharth, Wagdy Mohamed, Hamed Belal, Thakurathi Priyesh, Al-shammari Ali Saad
Anti-inflammatory regimen associated with reduced incidence of early homograft stenosis following the Ross procedureKhan Kathleen, Degraaff Dominique, Gray Mary Anne, Korukonda Samhita, Flodin Rachel, Degraaff Bret, Dhanekula Arjune, Deroo Scott, Burke Christopher