Final ID: MP1198
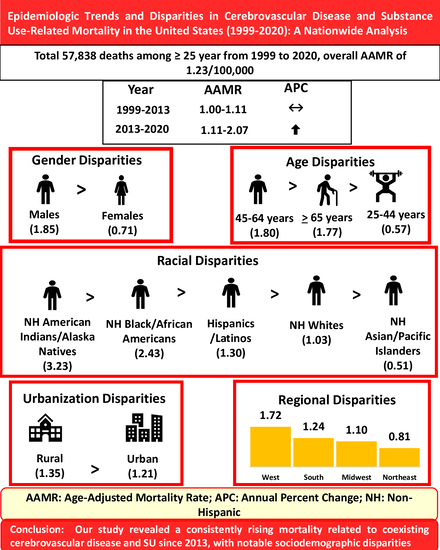
Epidemiologic Trends and Disparities in Cerebrovascular Disease and Substance Use-Related Mortality in the United States (1999-2020): A Nationwide Analysis
Abstract Body (Do not enter title and authors here):
Background
Substance use (SU) is a recognized risk factor for cerebrovascular disease, yet national mortality trends in affected populations remain underexplored. This study examines contemporary trends in mortality among adults (>25 years) in the United States with coexisting cerebrovascular diseases and substance use from 1999 to 2020.
Methods
We analyzed the mortality data using the CDC WONDER database, extracting age-adjusted mortality rates (AAMR) per 100,000 population. We used the respective ICD-10 codes to identify the fatalities where both cerebrovascular disease (I60–I69) and SU (E24.4, F10–F19, G31.2, G62.1, G72.1, I42.6, K70, K85.2, K86.0, R78.0–R78.4, T40, T42.3, T42.4, T42.6, T42.7, T43.6, T50.9, T51–T53, X61, X62, X64–X66, Y11, Y12, Y14–Y16) were either the underlying or contributing cause of death. We analyzed mortality trends by year, sex, race and ethnicity, census region, state, and metropolitan status. Joinpoint regression was used to calculate the annual percent change (APC) in AAMR with 95% confidence intervals.
Results
From 1999 to 2019, a total of 57,838 deaths occurred where the decedent had coexisting cerebrovascular disease and SU, with an overall AAMR of 1.23/100,000. The overall AAMR increased from 0.99 in 1999 to 2.07 in 2020, with a stable trend from 1999 to 2013 (APC: 0.28, p = 0.405), followed by a significantly rising trend from 2013 to 2020 (APC: 9.52, p < 0.001). Men had a higher AAMR (1.85) than women (0.71). American Indian or Alaska Native population had the highest AAMR (3.23), followed by Blacks or African Americans (2.43), Hispanics/Latinos (1.30), Whites (1.03), and Asians/Pacific Islanders (0.51). Significant geographical variations were observed, with the West region (1.72) and the District of Columbia (2.78) having the highest AAMR compared to others. Non-metropolitan areas had a higher AAMR (1.35) than metropolitan areas (1.21).
Conclusion
Our study revealed a consistently rising mortality related to concomitant cerebrovascular disease and SU since 2013, with notable sociodemographic disparities. These findings highlight SU as an important contributor to cerebrovascular mortality in the US.
Background
Substance use (SU) is a recognized risk factor for cerebrovascular disease, yet national mortality trends in affected populations remain underexplored. This study examines contemporary trends in mortality among adults (>25 years) in the United States with coexisting cerebrovascular diseases and substance use from 1999 to 2020.
Methods
We analyzed the mortality data using the CDC WONDER database, extracting age-adjusted mortality rates (AAMR) per 100,000 population. We used the respective ICD-10 codes to identify the fatalities where both cerebrovascular disease (I60–I69) and SU (E24.4, F10–F19, G31.2, G62.1, G72.1, I42.6, K70, K85.2, K86.0, R78.0–R78.4, T40, T42.3, T42.4, T42.6, T42.7, T43.6, T50.9, T51–T53, X61, X62, X64–X66, Y11, Y12, Y14–Y16) were either the underlying or contributing cause of death. We analyzed mortality trends by year, sex, race and ethnicity, census region, state, and metropolitan status. Joinpoint regression was used to calculate the annual percent change (APC) in AAMR with 95% confidence intervals.
Results
From 1999 to 2019, a total of 57,838 deaths occurred where the decedent had coexisting cerebrovascular disease and SU, with an overall AAMR of 1.23/100,000. The overall AAMR increased from 0.99 in 1999 to 2.07 in 2020, with a stable trend from 1999 to 2013 (APC: 0.28, p = 0.405), followed by a significantly rising trend from 2013 to 2020 (APC: 9.52, p < 0.001). Men had a higher AAMR (1.85) than women (0.71). American Indian or Alaska Native population had the highest AAMR (3.23), followed by Blacks or African Americans (2.43), Hispanics/Latinos (1.30), Whites (1.03), and Asians/Pacific Islanders (0.51). Significant geographical variations were observed, with the West region (1.72) and the District of Columbia (2.78) having the highest AAMR compared to others. Non-metropolitan areas had a higher AAMR (1.35) than metropolitan areas (1.21).
Conclusion
Our study revealed a consistently rising mortality related to concomitant cerebrovascular disease and SU since 2013, with notable sociodemographic disparities. These findings highlight SU as an important contributor to cerebrovascular mortality in the US.
More abstracts on this topic:
Cannabis Use In Adolescence Is Not Associated With Differences In BMI Z-Scores
Mahar Amy, Dusenbery Susan, Mittleman Murray
A pharmacist-led, population health approach to optimizing care in patients with hypertension and type II diabetes mellitus in minority groupsDoyle Julie, Haftel Elizabeth, Monroe Janet, Chen Zsu-zsu, Benson Mark, Yankama Tuyen, Adam Atif, Rubin Rochelle