Final ID: Mo1004
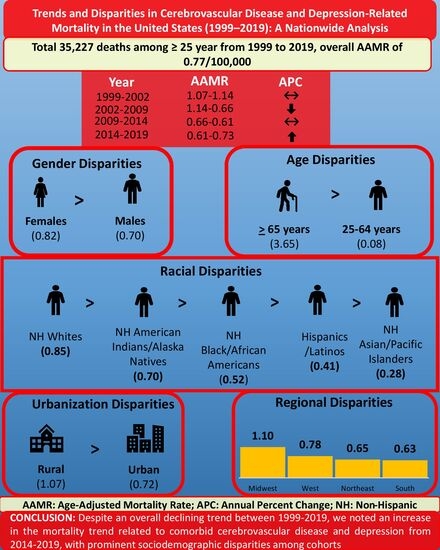
Trends and Disparities in Cerebrovascular Disease and Depression-Related Mortality in the United States (1999–2019): A Nationwide Analysis
Abstract Body (Do not enter title and authors here): Background
Clinical depression is associated with an increased risk of cerebrovascular accidents. Despite this risk, the mortality trends related to both depression and cerebrovascular disease have been unexplored. This study investigates contemporary mortality trends among U.S. adults (aged ≥25 years) with coexisting depression and cerebrovascular disease over the two decades spanning from 1999 to 2019.
Methods
We analyzed the death data using the CDC WONDER database. We extracted the age-adjusted mortality rates (AAMR) per 100,000 population from 1999 to 2019. We identified depression by using the ICD-10 codes F32, F33, F41.2, and F92.0. Cerebrovascular disease was identified using the ICD-10 codes I60-I69. Deaths with cerebrovascular disease and depression as either underlying or contributing causes were included in the study. Trends were analyzed by year, sex, race and ethnicity, census region, and metropolitan status. Joinpoint regression was used to calculate the annual percent change (APC) in AAMR with 95% confidence intervals (CI).
Results
During the study period, a total of 35,227 deaths occurred in patients with comorbid cerebrovascular disease and depression, with an overall AAMR of 0.77 per 100,000. The overall AAMR decreased from 1.07 in 1999 to 0.73 in 2019, was stable from 1999 to 2002 (APC: 1.63, p = 0.057), decreased from 2002 to 2009 (APC: -7.57, p < 0.001), remained stable from 2009 to 2014 (APC: -1.72, p = 0.111), and increased from 2014 to 2019 (APC: 3.46, p = 0.0004). Women had a higher AAMR (0.82) than men (0.70). Racial disparities showed that non-Hispanic (NH) Whites had the highest AAMR (0.85), followed by NH American Indian/Alaska Natives (0.70), NH Black/African Americans (0.52), Hispanics/Latinos (0.41), and NH Asians/Pacific Islanders (0.28). Significant geographic variation was also observed, with the Midwest region (1.1) and the state of Alabama (2.53) exhibiting the highest AAMR. Non-metropolitan areas had a higher AAMR (1.07) than metropolitan areas (0.72).
Conclusion
Despite an overall declining trend between 1999-2019, we noted an increase in the mortality trend related to comorbid cerebrovascular disease and depression from 2014-2019, with prominent sociodemographic disparities among cohorts. These findings highlight the importance of both neurological and psychological approaches in the management of cerebrovascular disease care, particularly among vulnerable sociodemographic groups.
Clinical depression is associated with an increased risk of cerebrovascular accidents. Despite this risk, the mortality trends related to both depression and cerebrovascular disease have been unexplored. This study investigates contemporary mortality trends among U.S. adults (aged ≥25 years) with coexisting depression and cerebrovascular disease over the two decades spanning from 1999 to 2019.
Methods
We analyzed the death data using the CDC WONDER database. We extracted the age-adjusted mortality rates (AAMR) per 100,000 population from 1999 to 2019. We identified depression by using the ICD-10 codes F32, F33, F41.2, and F92.0. Cerebrovascular disease was identified using the ICD-10 codes I60-I69. Deaths with cerebrovascular disease and depression as either underlying or contributing causes were included in the study. Trends were analyzed by year, sex, race and ethnicity, census region, and metropolitan status. Joinpoint regression was used to calculate the annual percent change (APC) in AAMR with 95% confidence intervals (CI).
Results
During the study period, a total of 35,227 deaths occurred in patients with comorbid cerebrovascular disease and depression, with an overall AAMR of 0.77 per 100,000. The overall AAMR decreased from 1.07 in 1999 to 0.73 in 2019, was stable from 1999 to 2002 (APC: 1.63, p = 0.057), decreased from 2002 to 2009 (APC: -7.57, p < 0.001), remained stable from 2009 to 2014 (APC: -1.72, p = 0.111), and increased from 2014 to 2019 (APC: 3.46, p = 0.0004). Women had a higher AAMR (0.82) than men (0.70). Racial disparities showed that non-Hispanic (NH) Whites had the highest AAMR (0.85), followed by NH American Indian/Alaska Natives (0.70), NH Black/African Americans (0.52), Hispanics/Latinos (0.41), and NH Asians/Pacific Islanders (0.28). Significant geographic variation was also observed, with the Midwest region (1.1) and the state of Alabama (2.53) exhibiting the highest AAMR. Non-metropolitan areas had a higher AAMR (1.07) than metropolitan areas (0.72).
Conclusion
Despite an overall declining trend between 1999-2019, we noted an increase in the mortality trend related to comorbid cerebrovascular disease and depression from 2014-2019, with prominent sociodemographic disparities among cohorts. These findings highlight the importance of both neurological and psychological approaches in the management of cerebrovascular disease care, particularly among vulnerable sociodemographic groups.
More abstracts on this topic:
A Quarter Century of Cardiovascular Risk: National Mortality Trends in Hypertension and Arrhythmias Among U.S. Adults Aged 55 and Older
Ahmad Husnain, Khan Muhammad, Sharif Aleena, Hossain Mohammad, Eltawansy Sherif, Faizan Muhammad, Ali Muhammad Faizan, Ahmed Ashraf, Abdul Malik Mohammad Hamza Bin, Pahwani Ritesh, Patel Rahul, Mehdi Hassan
A Meta-Analysis Comparing Same-Day Discharge to Later-Day Discharge in Transcatheter Aortic Valve ReplacementJain Hritvik, Passey Siddhant, Jain Jyoti, Goyal Aman, Wasir Amanpreet, Ahmed Mushood, Patel Nandan, Yadav Ashish, Shah Janhvi, Mehta Aryan