Final ID: MP2500
The Use of Common Cardiovascular Medications Is Associated With a Comparable Decreased Relative CVD Risk in Cancer Survivors and non-Cancer Patients
Abstract Body (Do not enter title and authors here): Introduction: The frequent coexistence of cardiovascular disease (CVD) and cancer, including due to shared risk factors, necessitates understanding the benefit of medications in CVD prevention in cancer survivors.
Hypothesis: We hypothesized that the use of statins, anti-hypertensives, and aspirin (ASA), provides equivalent CVD prevention for cancer and non-cancer patients for the same extent of CVD risk.
Methods: We used data from the Atherosclerosis Risk in Communities (ARIC) study, a cohort with 28 years of follow-up. After excluding those with prevalent cancer or CVD, the study population included 12,832 persons. Statin, anti-hypertensive, or ASA use was assessed by interview and bottle review at each study visit. Participants contributed time at risk of CVD until CVD diagnosis, cancer diagnosis, death, or administrative censoring, whichever came first. In the cancer survivor group, time at risk began at cancer diagnosis; participants with CVD diagnosed before cancer were excluded. Cox regression yielded the hazard ratio of CVD for medication use (time-varying) in those with and without cancer, adjusted for CVD risk factors*. As a sensitivity analysis and to increase the comparability of groups, Cox regression was performed on matched data where cancer and non-cancer participants were matched 1:1 using propensity scores based on clinical and demographic factors.
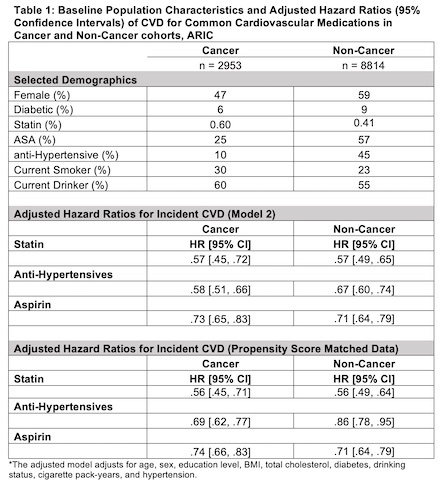
Results: Table 1 displays baseline characteristics between the cancer and non-cancer groups. The number of those who developed incident CVD in the non-cancer group was 3653 out of 8814 participants. The number of those who developed incident CVD in the cancer group was 877 out of 2953 participants. Table 1 also displays the results of the proportional hazards models, including those obtained after propensity score matching. Across both the unmatched and matched analyses, statins, anti-hypertensives, and ASA were all associated with a decreased risk of incident CVD in both cancer and non-cancer groups. The hazard ratios were comparable between the matched and unmatched analyses.
Conclusion: In this prospective study, statin, anti-hypertensive, and ASA use were associated with a comparable decreased CVD relative risk among those with and without cancer. This work suggests that cancer survivors may experience comparable CVD risk reduction benefit from these common medications.
Hypothesis: We hypothesized that the use of statins, anti-hypertensives, and aspirin (ASA), provides equivalent CVD prevention for cancer and non-cancer patients for the same extent of CVD risk.
Methods: We used data from the Atherosclerosis Risk in Communities (ARIC) study, a cohort with 28 years of follow-up. After excluding those with prevalent cancer or CVD, the study population included 12,832 persons. Statin, anti-hypertensive, or ASA use was assessed by interview and bottle review at each study visit. Participants contributed time at risk of CVD until CVD diagnosis, cancer diagnosis, death, or administrative censoring, whichever came first. In the cancer survivor group, time at risk began at cancer diagnosis; participants with CVD diagnosed before cancer were excluded. Cox regression yielded the hazard ratio of CVD for medication use (time-varying) in those with and without cancer, adjusted for CVD risk factors*. As a sensitivity analysis and to increase the comparability of groups, Cox regression was performed on matched data where cancer and non-cancer participants were matched 1:1 using propensity scores based on clinical and demographic factors.
Results: Table 1 displays baseline characteristics between the cancer and non-cancer groups. The number of those who developed incident CVD in the non-cancer group was 3653 out of 8814 participants. The number of those who developed incident CVD in the cancer group was 877 out of 2953 participants. Table 1 also displays the results of the proportional hazards models, including those obtained after propensity score matching. Across both the unmatched and matched analyses, statins, anti-hypertensives, and ASA were all associated with a decreased risk of incident CVD in both cancer and non-cancer groups. The hazard ratios were comparable between the matched and unmatched analyses.
Conclusion: In this prospective study, statin, anti-hypertensive, and ASA use were associated with a comparable decreased CVD relative risk among those with and without cancer. This work suggests that cancer survivors may experience comparable CVD risk reduction benefit from these common medications.
More abstracts on this topic:
A Polygenic Score to Identify Risk of Incident Stroke and Benefit from Primary Prevention Statin Therapy
Mcclintick Daniel, Kamanu Frederick, Melloni Giorgio, Sabatine Marc, Ruff Christian, Ridker Paul, Chasman Daniel, Marston Nicholas
A diagnostic challenge overcome with persistent clinical suspicion in a case of cardiac AL amyloidosisZimmerman Allison, Kuriakose Philip, Godfrey Amanda, Ananthasubramaniam Karthikeyan, Cowger Jennifer, Al-darzi Waleed