Final ID: MP325
A Diagnostic Challenge: Wild-Type Transthyretin Cardiac Amyloidosis in a Patient With Systemic Lupus and Ischemic Cardiomyopathy
Abstract Body (Do not enter title and authors here):
Background:
Transthyretin cardiac amyloidosis (ATTR-CM) is a progressive, infiltrative cardiomyopathy increasingly recognized in older adults. Despite improved awareness, and diagnostic modalities, diagnosis is often delayed due to symptom overlap with more common conditions. Patients with preexisting comorbidities, such as autoimmune disease or ischemic heart disease, are at even higher risk of diagnostic overshadowing. Herein, we describe a diagnostic conundrum of ATTR-CM in a patient with coexisting systemic lupus erythematosus (SLE) and Ischemic cardiomyopathy.
Case Description:
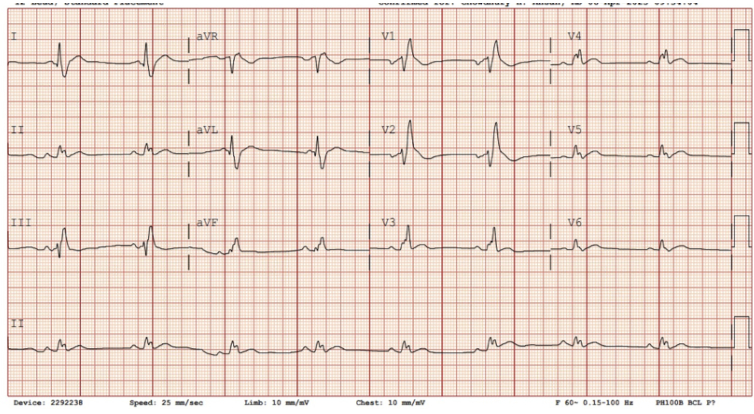
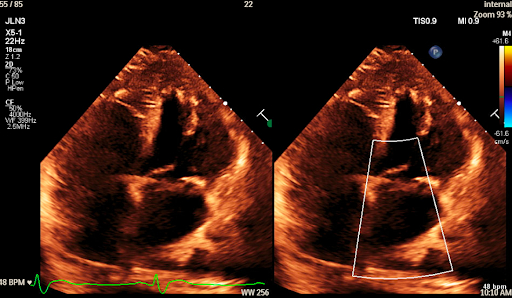
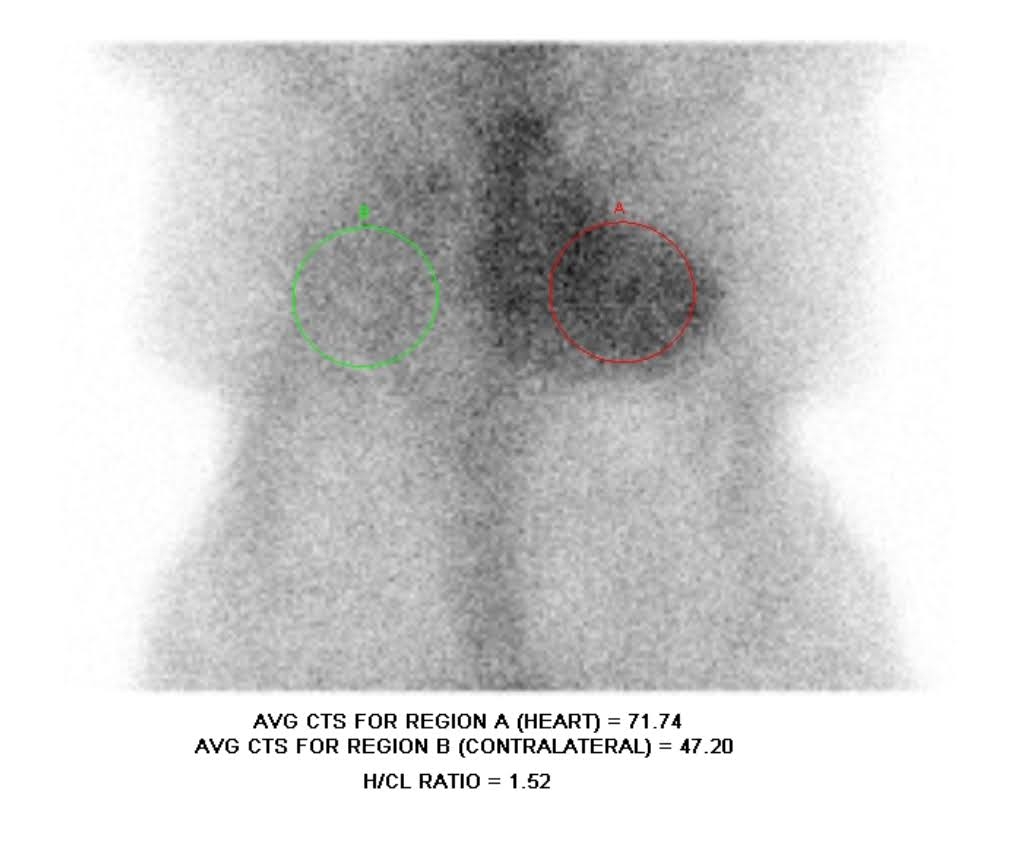
A 70-year-old female with coronary artery disease post-CABG, SLE with prior lupus nephritis and kidney transplant, and recurrent DVTs presented with dyspnea and bilateral leg edema. Her labs revealed macrocytic anemia, elevated NT-proBNP (41,167 pg/mL), and HS troponin-I (peak 689 ng/L). EKG showed sinus bradycardia, right bundle branch block, and low-voltage QRS complexes (Figure 1). Echocardiography demonstrated preserved ejection fraction of 55%, mild concentric LVH, and biatrial enlargement (Figure 2). Coronary angiography showed a mid-RCA lesion treated with PCI, but her symptoms persisted. The discordance between a low-voltage EKG and increased wall thickness on echocardiography raised suspicion of infiltrative cardiomyopathy. Serum and urine immunofixation and light chain analysis ruled out AL amyloidosis. A technetium-99m PYP scan showed grade 3 uptake with a heart-to-contralateral ratio of 1.52 (Figure 3). Genetic testing ruled out TTR mutation, confirming wild-type ATTR-CM. She was treated with cautious diuresis using lasix and referred for outpatient disease-modifying treatment.
Discussion:
This case highlights the diagnostic complexity of ATTR-CM in patients with overlapping cardiac and systemic comorbidities. Initial symptoms were attributed to ischemic and autoimmune causes, delaying recognition of amyloidosis. Red flags, such as disproportionate biomarker elevation, low-voltage EKG with LVH, and persistent symptoms despite intervention, prompted re-evaluation. . A stepwise non-invasive workup led to a timely, biopsy-free diagnosis. Early identification is critical, as novel disease-modifying therapies can significantly alter prognosis. This case highlights the importance of heightened clinical suspicion and awareness of ATTR-CM in patients with coexisting chronic disease states and overlapping symptomatology.
Background:
Transthyretin cardiac amyloidosis (ATTR-CM) is a progressive, infiltrative cardiomyopathy increasingly recognized in older adults. Despite improved awareness, and diagnostic modalities, diagnosis is often delayed due to symptom overlap with more common conditions. Patients with preexisting comorbidities, such as autoimmune disease or ischemic heart disease, are at even higher risk of diagnostic overshadowing. Herein, we describe a diagnostic conundrum of ATTR-CM in a patient with coexisting systemic lupus erythematosus (SLE) and Ischemic cardiomyopathy.
Case Description:
A 70-year-old female with coronary artery disease post-CABG, SLE with prior lupus nephritis and kidney transplant, and recurrent DVTs presented with dyspnea and bilateral leg edema. Her labs revealed macrocytic anemia, elevated NT-proBNP (41,167 pg/mL), and HS troponin-I (peak 689 ng/L). EKG showed sinus bradycardia, right bundle branch block, and low-voltage QRS complexes (Figure 1). Echocardiography demonstrated preserved ejection fraction of 55%, mild concentric LVH, and biatrial enlargement (Figure 2). Coronary angiography showed a mid-RCA lesion treated with PCI, but her symptoms persisted. The discordance between a low-voltage EKG and increased wall thickness on echocardiography raised suspicion of infiltrative cardiomyopathy. Serum and urine immunofixation and light chain analysis ruled out AL amyloidosis. A technetium-99m PYP scan showed grade 3 uptake with a heart-to-contralateral ratio of 1.52 (Figure 3). Genetic testing ruled out TTR mutation, confirming wild-type ATTR-CM. She was treated with cautious diuresis using lasix and referred for outpatient disease-modifying treatment.
Discussion:
This case highlights the diagnostic complexity of ATTR-CM in patients with overlapping cardiac and systemic comorbidities. Initial symptoms were attributed to ischemic and autoimmune causes, delaying recognition of amyloidosis. Red flags, such as disproportionate biomarker elevation, low-voltage EKG with LVH, and persistent symptoms despite intervention, prompted re-evaluation. . A stepwise non-invasive workup led to a timely, biopsy-free diagnosis. Early identification is critical, as novel disease-modifying therapies can significantly alter prognosis. This case highlights the importance of heightened clinical suspicion and awareness of ATTR-CM in patients with coexisting chronic disease states and overlapping symptomatology.
More abstracts on this topic:
Loeffler (Eosinophilic) Endocarditis Masquerading as Infective Endocarditis: Diagnostic Role of Multimodal Imaging
Bhagat Priyanka, Silva America, Afonso Luis
A Rare Association of Darier’s Disease and Dilated Cardiomyopathy: A Case Report Exploring the Cardiac Implications of ATP2A2 MutationJacob Nidhi