Final ID: Sa3022
Impact of Rural and Non-Rural Status on Congenital Heart Disease Healthcare Utilization and Outcomes
Abstract Body (Do not enter title and authors here): Introduction/Background: Congenital heart disease (CHD) is the leading cause of birth defects in the United States and contributes to billions of dollars in healthcare resource utilization each year. Rurality, as a social determinant of health, can exacerbate disparities in access to care, negatively impact the rate of prenatal detection of CHD, and increase healthcare resource utilization.
Research Question/Hypothesis: We hypothesized that patients living in rural areas would have lower rates of outpatient (OP) follow-up and higher rates of emergency department (ED) and inpatient (IP) hospital stays relative to patients living in urban or suburban areas.
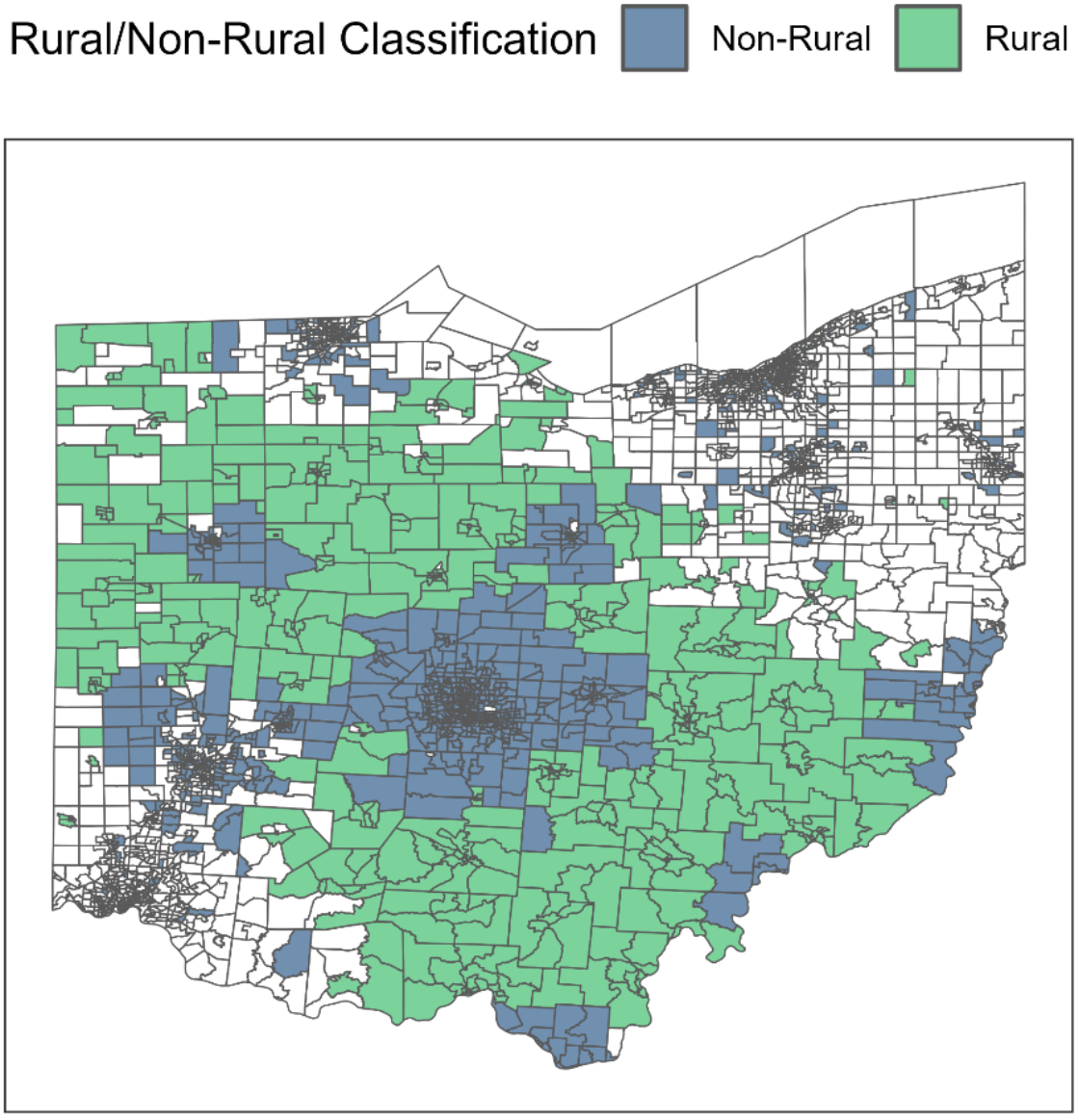
Methods/Approach: A retrospective cohort study of pediatric (0-17 years) CHD patients with an index visit at Nationwide Children’s Hospital (Columbus, OH) from 2013-2023 was conducted. Rurality was determined based on USDA Rural-Urban Commuting Area scores ≥ 4. Patients with at least one year of follow-up were retained for regression analysis of utilization rates. Quasi-Poisson regression models with offset terms were used to elucidate incidence rate ratios (IRR), 95% confidence intervals (CI), and p-values for utilization metrics. The log-rank test was used to compare mortality by rurality.
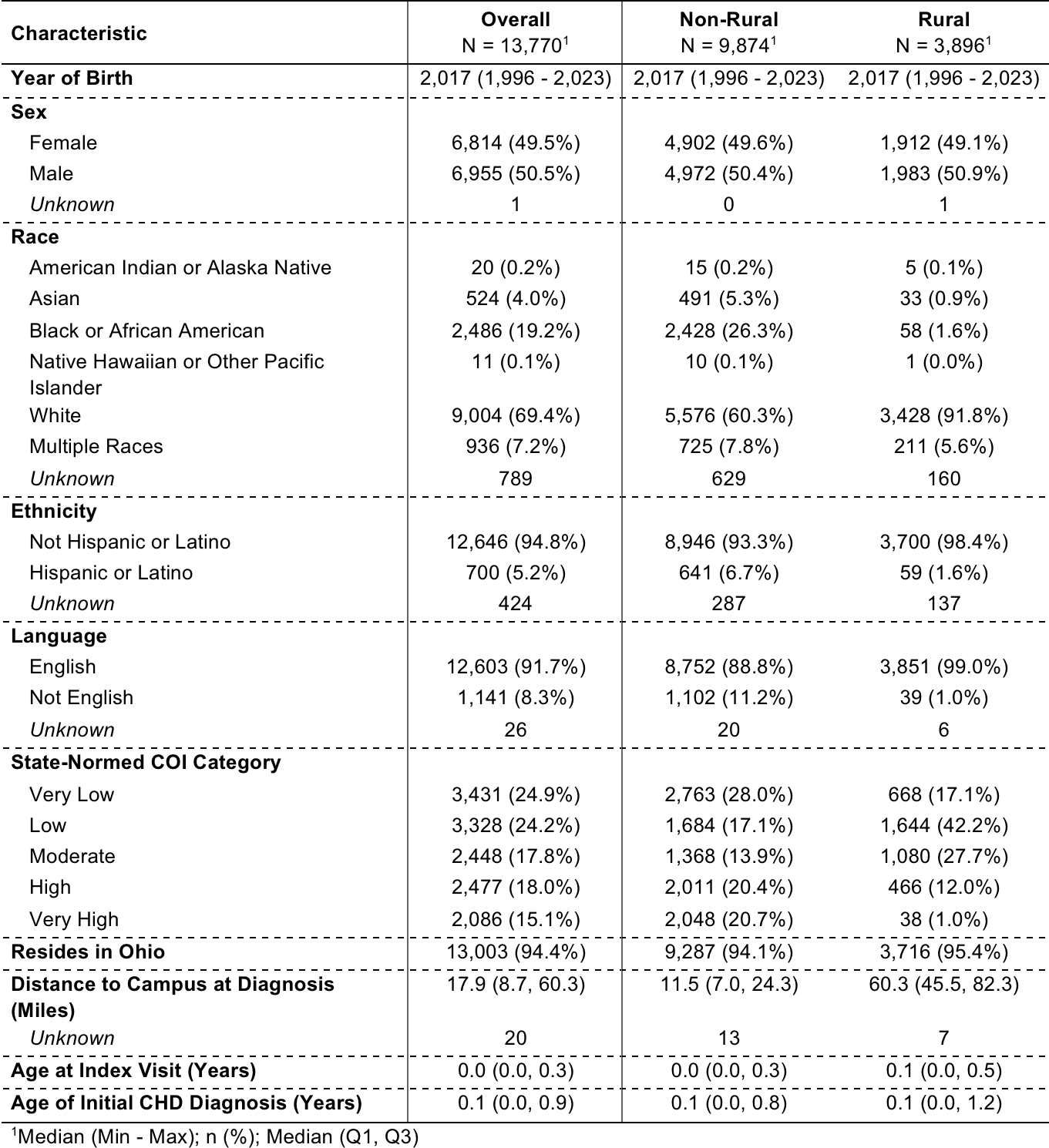
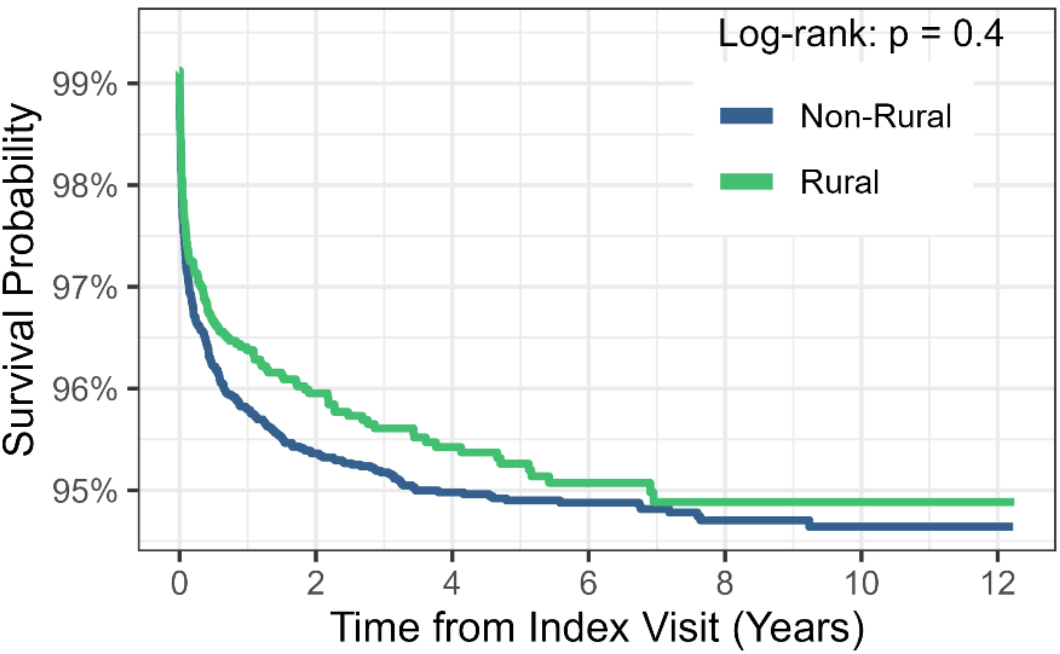
Results/Data: Of the 13,770 patients analyzed, 28.29% (3,896) were from rural areas. Patients from rural areas had an increased median driving distance at 60.3 miles versus 11.5 miles for those from non-rural areas. Rural patients additionally had a lower Child Opportunity Index (COI), as 59.3% (2,312) were considered “Low “or “Very Low” compared to 45.0% (4,447) of their non-rural counterparts. Rural patients had 1.23 (95% CI: 1.16, 1.30; p < 0.001) times the rate of OP cardiology visits, 0.58 (95% CI: 0.53, 0.62; p < 0.001) times the rate of ED visits, and no significant difference in rates of IP admissions (IRR = 1.04; 95% CI: 0.96, 1.13; p = 0.3) or mortality (log-rank p = 0.4) compared to non-rural patients.
Conclusions: Rural residency was associated with higher rates of OP cardiology visits, lower rates of ED visits, and similar rates of IP admissions and mortality. Limitations include lack of an all-payers claims database in our state, therefore only local records were utilized in this study. Future research could investigate the utilization of satellite clinics to further categorize OP cardiology visits by location.
Research Question/Hypothesis: We hypothesized that patients living in rural areas would have lower rates of outpatient (OP) follow-up and higher rates of emergency department (ED) and inpatient (IP) hospital stays relative to patients living in urban or suburban areas.
Methods/Approach: A retrospective cohort study of pediatric (0-17 years) CHD patients with an index visit at Nationwide Children’s Hospital (Columbus, OH) from 2013-2023 was conducted. Rurality was determined based on USDA Rural-Urban Commuting Area scores ≥ 4. Patients with at least one year of follow-up were retained for regression analysis of utilization rates. Quasi-Poisson regression models with offset terms were used to elucidate incidence rate ratios (IRR), 95% confidence intervals (CI), and p-values for utilization metrics. The log-rank test was used to compare mortality by rurality.
Results/Data: Of the 13,770 patients analyzed, 28.29% (3,896) were from rural areas. Patients from rural areas had an increased median driving distance at 60.3 miles versus 11.5 miles for those from non-rural areas. Rural patients additionally had a lower Child Opportunity Index (COI), as 59.3% (2,312) were considered “Low “or “Very Low” compared to 45.0% (4,447) of their non-rural counterparts. Rural patients had 1.23 (95% CI: 1.16, 1.30; p < 0.001) times the rate of OP cardiology visits, 0.58 (95% CI: 0.53, 0.62; p < 0.001) times the rate of ED visits, and no significant difference in rates of IP admissions (IRR = 1.04; 95% CI: 0.96, 1.13; p = 0.3) or mortality (log-rank p = 0.4) compared to non-rural patients.
Conclusions: Rural residency was associated with higher rates of OP cardiology visits, lower rates of ED visits, and similar rates of IP admissions and mortality. Limitations include lack of an all-payers claims database in our state, therefore only local records were utilized in this study. Future research could investigate the utilization of satellite clinics to further categorize OP cardiology visits by location.
More abstracts on this topic:
A Scoping Review Exploring Cardiovascular Risk and Health Metrics and Cancer Prediction
Kim Ji-eun, Henriquez Santos Gretell, Kumar Sant, Livinski Alicia, Vo Jacqueline, Joo Jungnam, Shearer Joe, Hashemian Maryam, Roger Veronique
Advanced Complementary Imaging Analysis of Single Ventricle Patients Using Cardiac Magnetic Resonance and EchocardiographyNaum Athanasios, Loke Yue-hin, Meyers Brett, Payne Ronald, Vlachos Pavlos