Final ID: MP1976
Timing and outcomes of staged coronary artery bypass grafting following percutaneous coronary intervention for STEMI – when should we intervene?
Abstract Body (Do not enter title and authors here): Introduction: While recommendations exist to guide timing of coronary artery bypass grafting (CABG) following STEMI, the optimal timing of staged CABG following percutaneous coronary intervention (PCI) for STEMI is unclear. Our aim is to utilize national claims data to assess national practice patterns for the timing of staged CABG following PCI for STEMI, predictors of timing and patient presentation, and the association of timing with post-operative outcomes.
Methods: Inpatient Medicare MedPAR files were reviewed to identify patients aged ≥65 years who underwent isolated CABG from 10/2016-12/2021, who underwent urgent PCI for STEMI within the 12-months prior to CABG. Patients with a diagnosis of in-stent restenosis were excluded, isolating patients undergoing CABG for residual native disease. Timing of CABG relative to PCI was identified as same admission, elective readmission, and urgent readmission. The primary endpoint was five-year survival, assessed using propensity-matched Kaplan-Meier analysis with log-rank test, and Cox proportional hazards models. Comparison groups included same admission versus elective readmission, and elective versus urgent readmission. Among patients readmitted for CABG, predictors of presenting urgently were assessed utilizing logistic regression analysis.
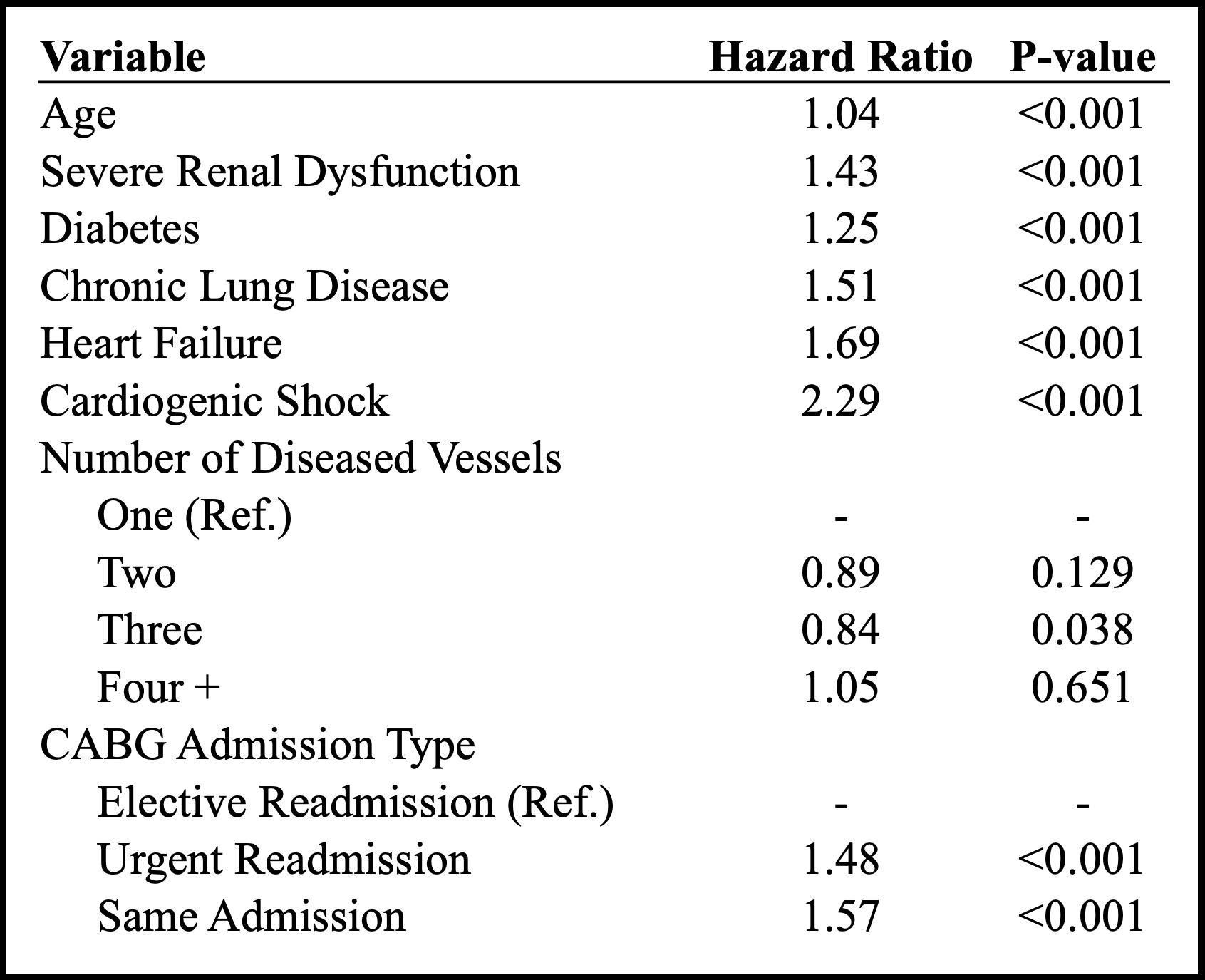
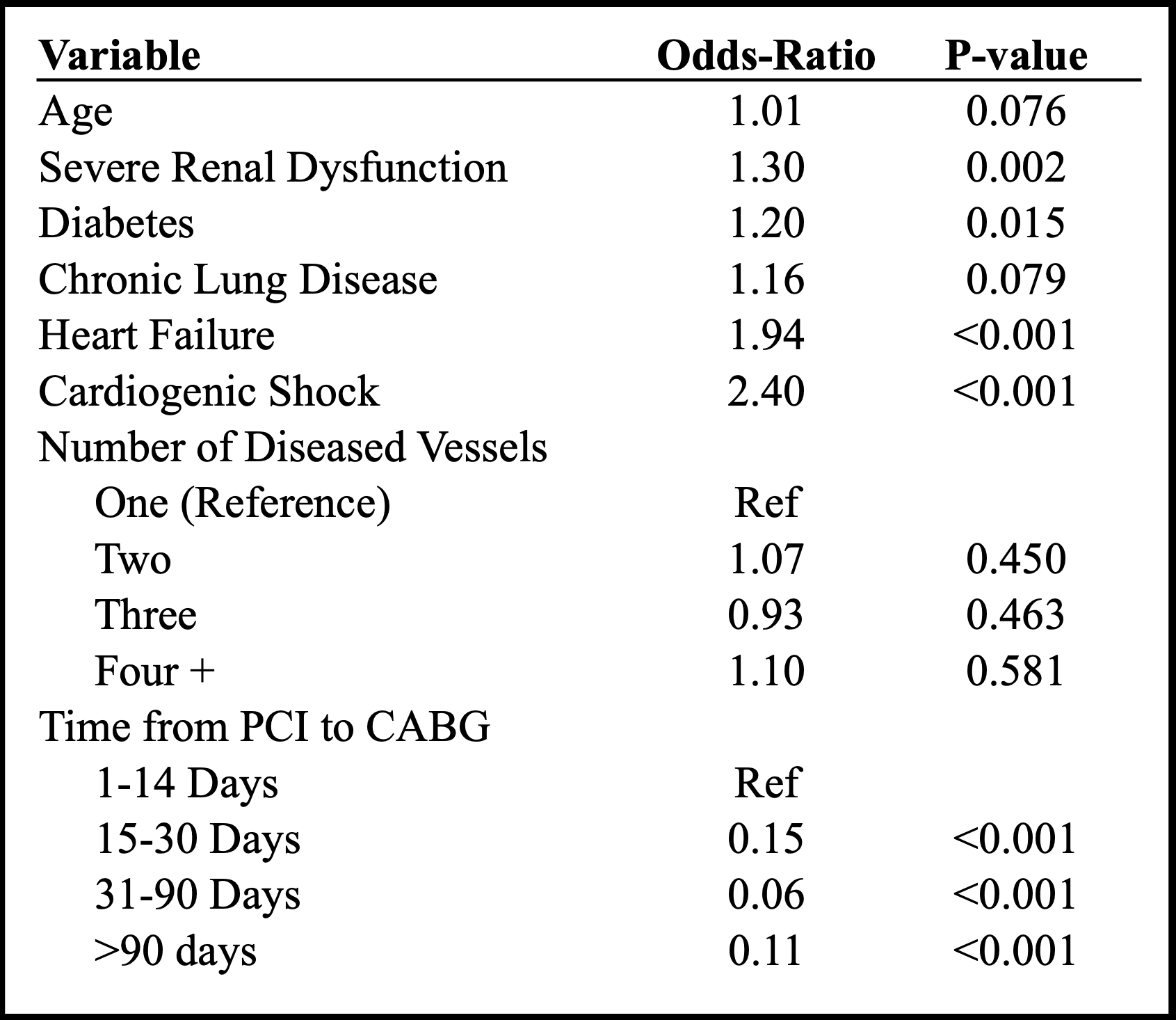
Results: During the study period, 428,867 patients underwent isolated CABG; of those, 14,652 (3.4%) underwent urgent PCI for ACS in the 12-months prior to CABG. After excluding patients with in-stent stenosis and NSTEMI diagnosis, the final cohort consisted of 7,792 STEMI patients who underwent CABG within 12-months of PCI for residual native disease. Among this cohort, 3,532 (45.3%) had CABG during the same admission as PCI, 2,805 (36.0%) returned for elective CABG, and 1,466 (18.8%) returned urgently for CABG. Patients undergoing same admission CABG had inferior five-year survival than those readmitted electively; however, patients readmitted urgently also had significantly reduced five-year survival (Figure 1, Table 1). Patients with increased comorbidity burden were more likely to be re-admitted urgently for CABG, with the highest risk ≤14 days post-PCI (Table 2).
Conclusion: Among patients who undergo PCI for STEMI with residual coronary disease requiring CABG, optimal outcomes are observed in the setting of discharge and elective readmission; however, risk of disease progression and urgent readmission for revascularization must be weighed carefully.
Methods: Inpatient Medicare MedPAR files were reviewed to identify patients aged ≥65 years who underwent isolated CABG from 10/2016-12/2021, who underwent urgent PCI for STEMI within the 12-months prior to CABG. Patients with a diagnosis of in-stent restenosis were excluded, isolating patients undergoing CABG for residual native disease. Timing of CABG relative to PCI was identified as same admission, elective readmission, and urgent readmission. The primary endpoint was five-year survival, assessed using propensity-matched Kaplan-Meier analysis with log-rank test, and Cox proportional hazards models. Comparison groups included same admission versus elective readmission, and elective versus urgent readmission. Among patients readmitted for CABG, predictors of presenting urgently were assessed utilizing logistic regression analysis.
Results: During the study period, 428,867 patients underwent isolated CABG; of those, 14,652 (3.4%) underwent urgent PCI for ACS in the 12-months prior to CABG. After excluding patients with in-stent stenosis and NSTEMI diagnosis, the final cohort consisted of 7,792 STEMI patients who underwent CABG within 12-months of PCI for residual native disease. Among this cohort, 3,532 (45.3%) had CABG during the same admission as PCI, 2,805 (36.0%) returned for elective CABG, and 1,466 (18.8%) returned urgently for CABG. Patients undergoing same admission CABG had inferior five-year survival than those readmitted electively; however, patients readmitted urgently also had significantly reduced five-year survival (Figure 1, Table 1). Patients with increased comorbidity burden were more likely to be re-admitted urgently for CABG, with the highest risk ≤14 days post-PCI (Table 2).
Conclusion: Among patients who undergo PCI for STEMI with residual coronary disease requiring CABG, optimal outcomes are observed in the setting of discharge and elective readmission; however, risk of disease progression and urgent readmission for revascularization must be weighed carefully.
More abstracts on this topic:
An Unusual Presentation of Cerebellar Stroke Following the Removal of Microaxial Flow Pump
Liu Zi Qian, Alsheikh-kassim Mohammad, Karpenos Joseph, Frodey Kevin
Artificial Intelligence ECG-Extracted Features Predict Microvascular Obstruction in ST-segment Elevation Myocardial InfarctionTraverse Jay, Meyers Pendell, Sharkey Scott, Schwager Sarah, Stanberry Larissa, Herman Robert