Final ID: MP1639
Early Re-Initiation of Optimal Guideline-Directed Medical Therapy after Coronary Artery Bypass Grafting in Patients with Heart Failure with Reduced Ejection is Associated with Decreased Mortality
Abstract Body (Do not enter title and authors here): Introduction: Guideline-directed medical therapy (GDMT) improves survival in medical patients with heart failure with reduced ejection fraction (HFrEF). For cardiac surgical patients with HFrEF, GDMT is typically held perioperatively; re-introduction may be hampered by post-operative frailty and vasoplegia. This study sought to examine patterns of GDMT prescription after coronary artery bypass grafting (CABG) in patients with HFrEF and baseline optimal medical therapy, and the potential benefit of return to optimal dosing.
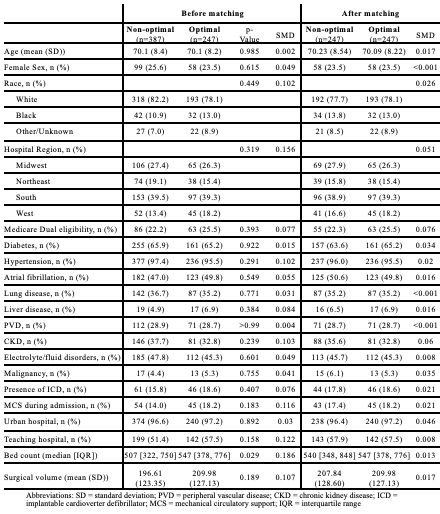
Methods: The population included Medicare beneficiaries who underwent isolated CABG from 2016-2019, with a HFrEF diagnosis in the prior 6 months, on baseline optimal GDMT as characterized by the Heart Failure Collaboratory score, which standardizes across medication classes and doses. Prescription patterns were evaluated across patients who did and did not achieve optimal GDMT by 90 days post-discharge (defined as a score of ≥4 with both beta-blocker and renin-angiotensin-aldosterone inhibitor (RAASi) prescription). Via propensity score matching, a Cox proportional hazard model was applied to compare all-cause mortality and a composite of mortality and HF readmission between the optimal and non-optimal cohorts.
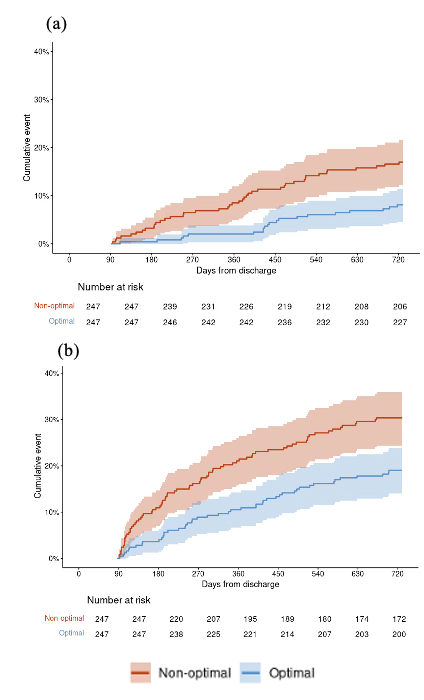
Results: Of the 634 patients meeting inclusion criteria, 247 (39.0%) were re-initiated on optimal GDMT within 90 days of discharge. Mineralocorticoid receptor antagonists (MRAs) represented the class with the lowest uptake in both the non-optimal and optimal cohorts (17.1% and 70.0%) (Figure 1). Angiotensin receptor-neprilysin inhibitor (ARNI) use was scarce, representing 33.6% of RAASi in the optimal cohort and <5% in the non-optimal cohort. Cohorts were similar at baseline, although optimal patients were more likely to have had surgery at larger hospitals (Table 1). After matching, the optimal group demonstrated significantly decreased hazard of mortality (8.1% vs. 17.0%; HR 0.45 [0.25-0.76], p=0.002) and composite of mortality and HF readmission at 2 years (19.0% vs. 30.4%; HR 0.57 [0.40-0.82], p=0.003) (Figure 2).
Conclusion: Patients with HFrEF on optimal GDMT at baseline who undergo CABG and are re-initiated on an optimal regimen within 90 days of discharge had significantly decreased risk of mortality and heart failure readmission. These findings highlight a need to identify barriers to GDMT after cardiac surgery such that these patients may benefit long-term from the combined effects of surgical and medical optimization.
Methods: The population included Medicare beneficiaries who underwent isolated CABG from 2016-2019, with a HFrEF diagnosis in the prior 6 months, on baseline optimal GDMT as characterized by the Heart Failure Collaboratory score, which standardizes across medication classes and doses. Prescription patterns were evaluated across patients who did and did not achieve optimal GDMT by 90 days post-discharge (defined as a score of ≥4 with both beta-blocker and renin-angiotensin-aldosterone inhibitor (RAASi) prescription). Via propensity score matching, a Cox proportional hazard model was applied to compare all-cause mortality and a composite of mortality and HF readmission between the optimal and non-optimal cohorts.
Results: Of the 634 patients meeting inclusion criteria, 247 (39.0%) were re-initiated on optimal GDMT within 90 days of discharge. Mineralocorticoid receptor antagonists (MRAs) represented the class with the lowest uptake in both the non-optimal and optimal cohorts (17.1% and 70.0%) (Figure 1). Angiotensin receptor-neprilysin inhibitor (ARNI) use was scarce, representing 33.6% of RAASi in the optimal cohort and <5% in the non-optimal cohort. Cohorts were similar at baseline, although optimal patients were more likely to have had surgery at larger hospitals (Table 1). After matching, the optimal group demonstrated significantly decreased hazard of mortality (8.1% vs. 17.0%; HR 0.45 [0.25-0.76], p=0.002) and composite of mortality and HF readmission at 2 years (19.0% vs. 30.4%; HR 0.57 [0.40-0.82], p=0.003) (Figure 2).
Conclusion: Patients with HFrEF on optimal GDMT at baseline who undergo CABG and are re-initiated on an optimal regimen within 90 days of discharge had significantly decreased risk of mortality and heart failure readmission. These findings highlight a need to identify barriers to GDMT after cardiac surgery such that these patients may benefit long-term from the combined effects of surgical and medical optimization.
More abstracts on this topic:
A Rare Cause of Recurrent Heart Failure Exacerbations After Transcatheter Aortic Valve Replacement: Ventricular Septal Defect and Significant Paravalvular Leak
Medina Jesse, Vincent Louis, Rodriguez Ferreira Esteban, Spence-miller Shanice, Fernandez Joel, Colombo Rosario, Calfa Marian
A Pilot Study of Post-Discharge Atrial Fibrillation Using a Novel Mobile Electrocardiography Monitoring DeviceIribarne Alexander, Kramer Robert, Moquete Ellen, Hupf Jonathan, Duncan Prezley, Mihelis Efstathia, Borger Michael, Muir Andrew, Starnes Vaughn, Edegran Albin, Fenton Kathleen, Patel Nirav, Taddei-peters Wendy, Moskowitz Alan, Ogara Patrick, Gelijns Annetine, Alexander John, Gillinov A, Bagiella Emilia, D'alessandro David, Dimaio John, Bhavnani Sanjeev, Badhwar Vinay, Sengupta Partho, Johnson Linda, Gajewska-dendek Elzbieta