Final ID: MP1991
Prognostic value of D-dimer and its incremental value in risk stratification models for atrial fibrillation patients with acute coronary syndrome or percutaneous coronary intervention
Abstract Body (Do not enter title and authors here): Background: Despite optimal medical therapy, patients with acute coronary syndrome (ACS) or undergoing percutaneous coronary intervention (PCI) still experience higher risk of thrombosis and bleeding events. However, more thrombus burden occurs in those complicated with atrial fibrillation (AF), leading to more difficult risk stratification and selection of anti-thrombotic strategies. D-dimer is a sensitive biomarker for thrombosis, but no research has evaluated its prognostic value in such extremely high-risk patients.
Objective: To investigate whether D-dimer could predict 1-year adverse events and improve the predictive value of CHA2DS2-VA score and HAS-BLED score in AF patients with ACS or PCI.
Methods: 2,182 consecutive AF patients with ACS or PCI at Fuwai Hospital from 2017 to 2019 were enrolled. Patients with in-hospital death, missing D-dimer data, or lost to follow-up were excluded. The optimal cut-off value of D-dimer was 0.53 according to the receiver operating curve. The primary endpoint was major adverse cardiovascular and cerebrovascular event (MACCE, including all-cause death, myocardial infarction, ischemic-driven revascularization, stroke or systemic embolism). The secondary endpoints were the composition of MACCE and bleeding events according to Thrombolysis in Myocardial Infarction criteria.
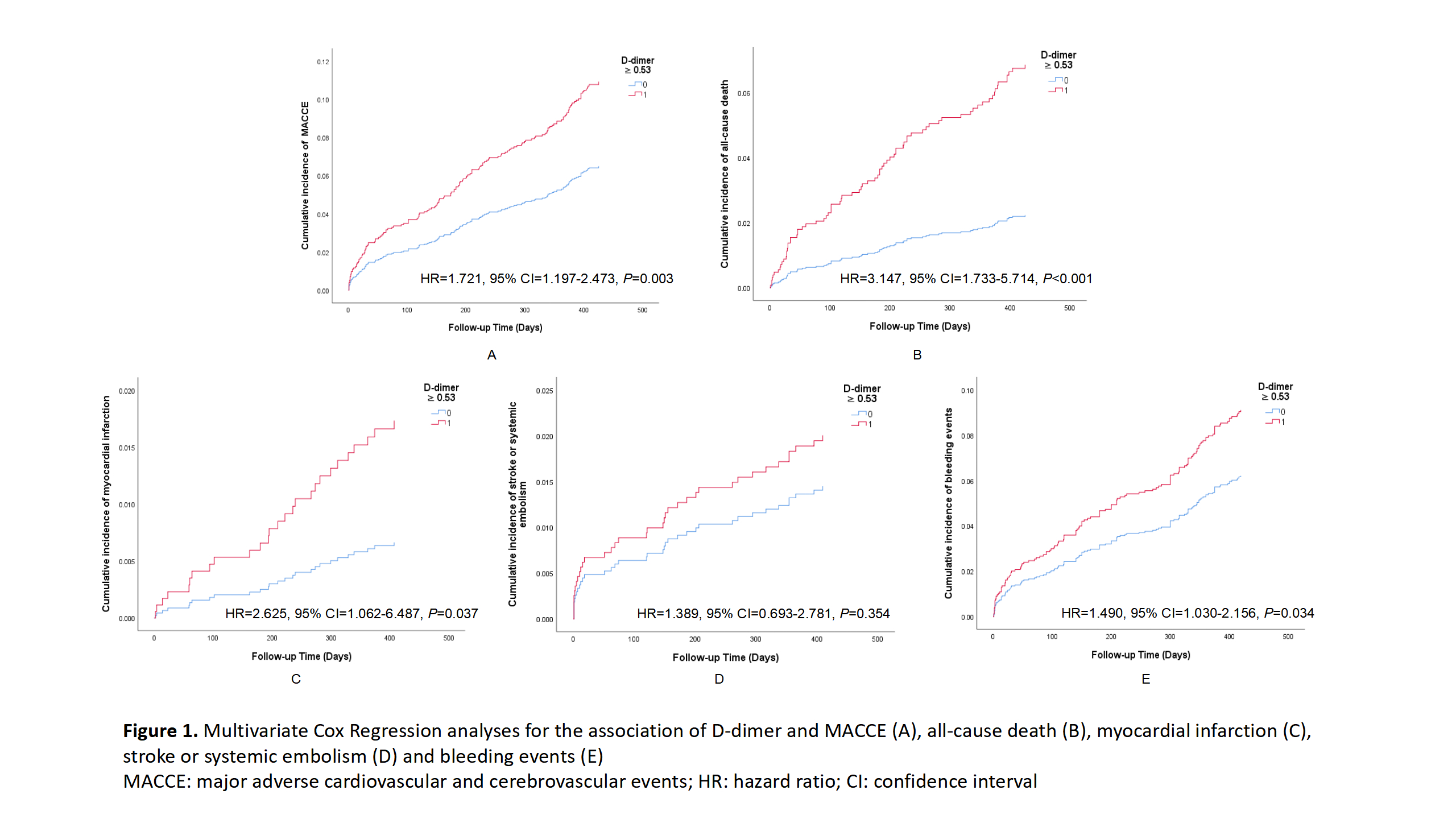
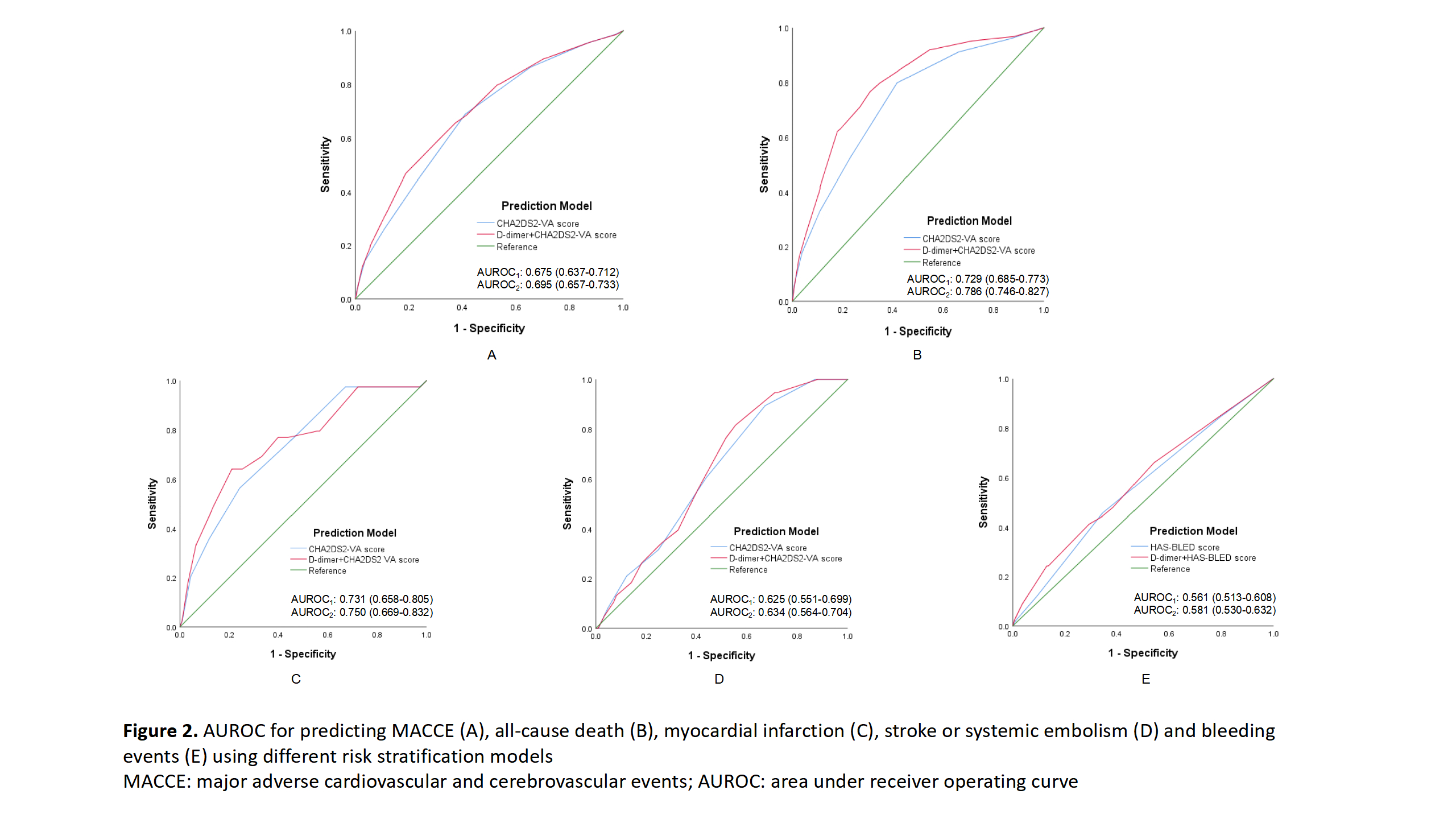
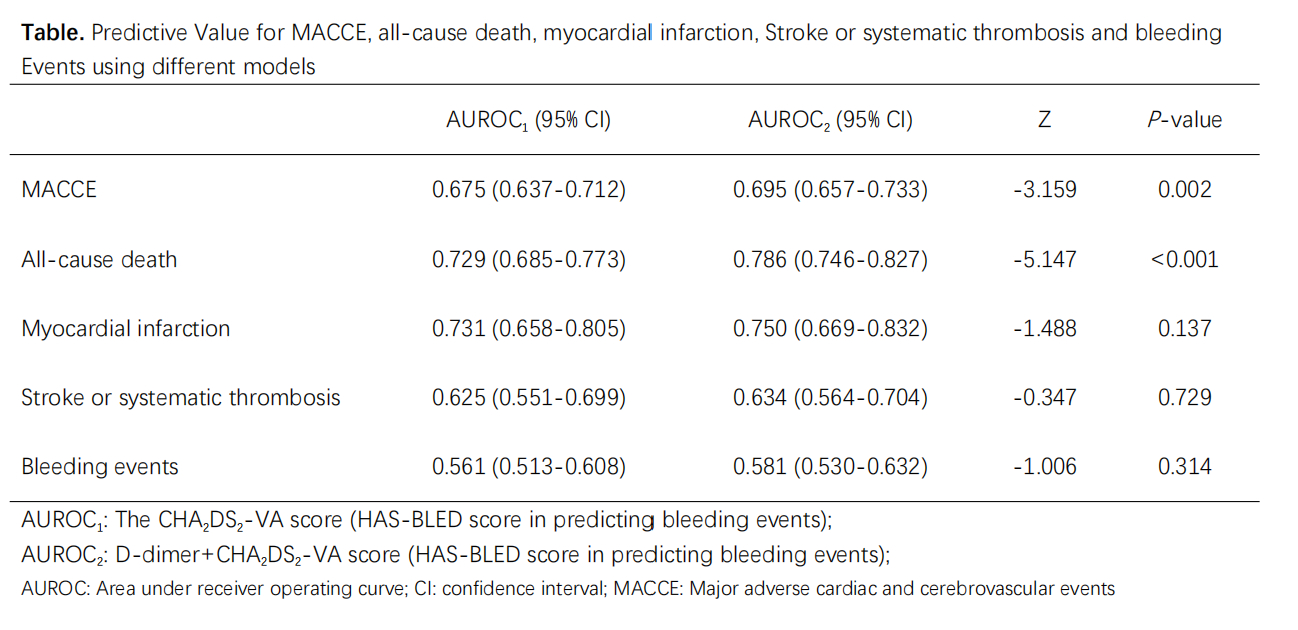
Results: Finally, 1,816 patients were included for analysis. After 1-year follow-up, 214 (11.8%) MACCE occurred. Multivariate Cox regression analysis suggested that D-dimer was the independent factor for MACCE (HR=1.721, 95% CI=1.197-2.473, P=0.003), all-cause death (HR=3.147, 95% CI=1.733-5.714, P<0.001), myocardial infarction (HR=2.625, 95% CI=1.062-6.487, P=0.037) and bleeding events (HR=1.490, 95% CI=1.030-2.156, P=0.034), but not for stroke or systemic embolism (Figure 1). After Combining with D-dimer, the predictive value of the CHA2DS2-VA score was significantly improved for MACCE (Area Under Curve [AUC] from 0.675 to 0.695, Z=-3.159, P=0.002) and all-cause death (AUC from 0.729 to 0.786, Z=-5.147, P<0.001), but not statistically significant for other events and HAS-BLED score (Figure 2 and Table).
Conclusions: For AF patients with ACS or PCI, D-dimer significantly predicted 1-year adverse events and improved the predictive value of CHA2DS2-VA score for MACCE and all-cause death. In the future, whether D-dimer could guide individualized anti-thrombotic therapy in such extremely high-risk patients deserves further investigation.
Objective: To investigate whether D-dimer could predict 1-year adverse events and improve the predictive value of CHA2DS2-VA score and HAS-BLED score in AF patients with ACS or PCI.
Methods: 2,182 consecutive AF patients with ACS or PCI at Fuwai Hospital from 2017 to 2019 were enrolled. Patients with in-hospital death, missing D-dimer data, or lost to follow-up were excluded. The optimal cut-off value of D-dimer was 0.53 according to the receiver operating curve. The primary endpoint was major adverse cardiovascular and cerebrovascular event (MACCE, including all-cause death, myocardial infarction, ischemic-driven revascularization, stroke or systemic embolism). The secondary endpoints were the composition of MACCE and bleeding events according to Thrombolysis in Myocardial Infarction criteria.
Results: Finally, 1,816 patients were included for analysis. After 1-year follow-up, 214 (11.8%) MACCE occurred. Multivariate Cox regression analysis suggested that D-dimer was the independent factor for MACCE (HR=1.721, 95% CI=1.197-2.473, P=0.003), all-cause death (HR=3.147, 95% CI=1.733-5.714, P<0.001), myocardial infarction (HR=2.625, 95% CI=1.062-6.487, P=0.037) and bleeding events (HR=1.490, 95% CI=1.030-2.156, P=0.034), but not for stroke or systemic embolism (Figure 1). After Combining with D-dimer, the predictive value of the CHA2DS2-VA score was significantly improved for MACCE (Area Under Curve [AUC] from 0.675 to 0.695, Z=-3.159, P=0.002) and all-cause death (AUC from 0.729 to 0.786, Z=-5.147, P<0.001), but not statistically significant for other events and HAS-BLED score (Figure 2 and Table).
Conclusions: For AF patients with ACS or PCI, D-dimer significantly predicted 1-year adverse events and improved the predictive value of CHA2DS2-VA score for MACCE and all-cause death. In the future, whether D-dimer could guide individualized anti-thrombotic therapy in such extremely high-risk patients deserves further investigation.
More abstracts on this topic:
A Randomized Clinical Trial Evaluating Vitamin D Normalization on Major Adverse Cardiovascular-Related Events Among Acute Coronary Syndrome Patients: The TARGET-D Trial
May Heidi, Colipi Dominique, Whiting Tyler, Muhlestein Joseph, Le Viet, Anderson Jeffrey, Babcock Daniel, Wayman Libby, Bair Tami, Knight Stacey, Knowlton Kirk, Iverson Leslie
A Comparative Analysis of Esophageal Cooling for Preventing Esophageal Injury Post Atrial Fibrillation Catheter Ablation: A Systematic Review and Meta-analysisIbrahim Momen Mohamed, Al Hennawi Hussam, Tanas Yousef, Abourady Youmna, Sewedan Nourhan, Hashem Ahmed Magdy, Motawea Karam R.