Final ID: MP2370
Persistent Focal Atrial Tachycardia In A Young Pregnant Woman: When Stability Isn’t Safe
Abstract Body (Do not enter title and authors here): A 23-year-old woman at 28 weeks of gestation with a childhood history of SVT managed with beta-blockers and no follow-up presented with sudden-onset palpitations, dyspnea, and fatigue.
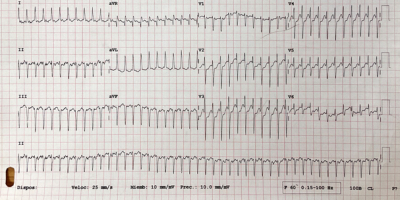
Initial ECG showed narrow complex tachycardia at 268 bpm, absent P waves, and left axis deviation. Differential diagnoses included PSVT, FAT, AVNRT, and AVRT.
She became asymptomatic after admission. Management included two doses of adenosine with transient effect, and escalating doses of metoprolol and propafenone with partial response. TTE revealed biatrial enlargement and diastolic dysfunction. Serial ECGs confirmed arrhythmia persistence. Fetal ultrasound was reassuring.
After seven days without rhythm control, she underwent zero-fluoroscopy catheter ablation with CARTO mapping. A microreentrant focus was identified between the right superior pulmonary vein and superior vena cava, confirming FAT. No complications occurred.
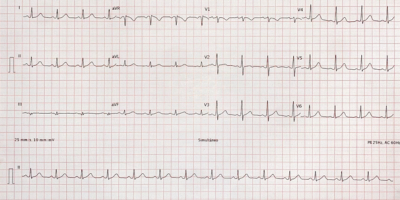
She was discharged in sinus rhythm at 90 bpm on metoprolol and propafenone. Follow-up showed no recurrence.
Pregnancy is a proarrhythmic state due to increased cardiac output, sympathetic tone, and atrial stretch. Hemodynamic stability does not rule out risk: Wang et al. reported 67% of pregnant women with FAT developed tachycardia-induced cardiomyopathy, many without overt instability. Guidelines recommend structural assessment and early intervention if HR exceeds 130 bpm, even in asymptomatic patients.
Despite normotension, persistent dyspnea, fatigue, and tachycardia >48 hours could have justified cardioversion, which is safe during all trimesters. Although a multidisciplinary team chose ablation, earlier cardioversion might have prevented atrial remodeling.
FAT in pregnancy remains underrecognized despite its potential to cause persistent symptoms and remodeling. Unlike AVNRT or AVRT, FAT is usually driven by abnormal automaticity, often incessant and unresponsive to vagal maneuvers or drugs. In >75% of reviewed cases, FAT was persistent or recurrent, often requiring multiple agents before ablation.
Zero-fluoroscopy ablation is safe and effective. A prospective study of 47 pregnant patients showed 100% acute success, no 24-month recurrence, and favorable obstetric outcomes.
Multidisciplinary care improves outcomes in pregnant patients with arrhythmias, where coordination among electrophysiology, cardiology, and obstetrics is essential for timely and individualized decision-making.
Initial ECG showed narrow complex tachycardia at 268 bpm, absent P waves, and left axis deviation. Differential diagnoses included PSVT, FAT, AVNRT, and AVRT.
She became asymptomatic after admission. Management included two doses of adenosine with transient effect, and escalating doses of metoprolol and propafenone with partial response. TTE revealed biatrial enlargement and diastolic dysfunction. Serial ECGs confirmed arrhythmia persistence. Fetal ultrasound was reassuring.
After seven days without rhythm control, she underwent zero-fluoroscopy catheter ablation with CARTO mapping. A microreentrant focus was identified between the right superior pulmonary vein and superior vena cava, confirming FAT. No complications occurred.
She was discharged in sinus rhythm at 90 bpm on metoprolol and propafenone. Follow-up showed no recurrence.
Pregnancy is a proarrhythmic state due to increased cardiac output, sympathetic tone, and atrial stretch. Hemodynamic stability does not rule out risk: Wang et al. reported 67% of pregnant women with FAT developed tachycardia-induced cardiomyopathy, many without overt instability. Guidelines recommend structural assessment and early intervention if HR exceeds 130 bpm, even in asymptomatic patients.
Despite normotension, persistent dyspnea, fatigue, and tachycardia >48 hours could have justified cardioversion, which is safe during all trimesters. Although a multidisciplinary team chose ablation, earlier cardioversion might have prevented atrial remodeling.
FAT in pregnancy remains underrecognized despite its potential to cause persistent symptoms and remodeling. Unlike AVNRT or AVRT, FAT is usually driven by abnormal automaticity, often incessant and unresponsive to vagal maneuvers or drugs. In >75% of reviewed cases, FAT was persistent or recurrent, often requiring multiple agents before ablation.
Zero-fluoroscopy ablation is safe and effective. A prospective study of 47 pregnant patients showed 100% acute success, no 24-month recurrence, and favorable obstetric outcomes.
Multidisciplinary care improves outcomes in pregnant patients with arrhythmias, where coordination among electrophysiology, cardiology, and obstetrics is essential for timely and individualized decision-making.
More abstracts on this topic:
Adipose tissue extracellular vesicles mediate pro-arrhythmic changes in atrial cardiomyocytes
Limpitikul Worawan, Garcia Contreras Marta, Betti Michael, Sheng Quanhu, Xiao Ling, Chatterjee Emeli, Gamazon Eric, Shah Ravi, Das Saumya
4D Cardiac Optogenetics Enable Complex Arrhythmia Modelling and Precise Interventional SimulationWexler Yehuda, Grinstein Harel, Landesberg Michal, Glatstein Shany, Huber Irit, Arbel Gil, Gepstein Lior