Final ID: Sa3108
Comparative Cardiovascular Outcomes in Acalabrutinib vs Zanubrutinib in B-Cell Malignancies: A TriNetX Data Study
Abstract Body (Do not enter title and authors here): Background:
Next-generation Bruton’s tyrosine kinase inhibitors (BTKis) such as acalabrutinib and
zanubrutinib have improved treatment outcomes in B-cell malignancies including chronic
lymphocytic leukemia (CLL), mantle cell lymphoma (MCL), and Waldenström
macroglobulinemia (WM), while reducing off-target toxicities compared to ibrutinib. However,
their comparative cardiovascular safety profiles remain poorly characterized. This study
evaluates real-world cardiovascular and clinical outcomes between zanubrutinib and
acalabrutinib using a large multi-center database.
Methods:
We conducted a retrospective cohort study using the TriNetX Research Network (October 2017–
December 2024) including adult patients with CLL, MCL, WM, or small B-cell lymphoma
treated with zanubrutinib or acalabrutinib. Patients with prior exposure to other BTKis were
excluded. After 1:1 propensity score matching, 2,363 patients were included in each cohort. We
assessed 3-year outcomes: new-onset atrial fibrillation/flutter, cerebral infarction, hypertension,
and all-cause mortality using odds ratios (ORs), Kaplan-Meier survival analysis, and log-rank
testing.
Results:
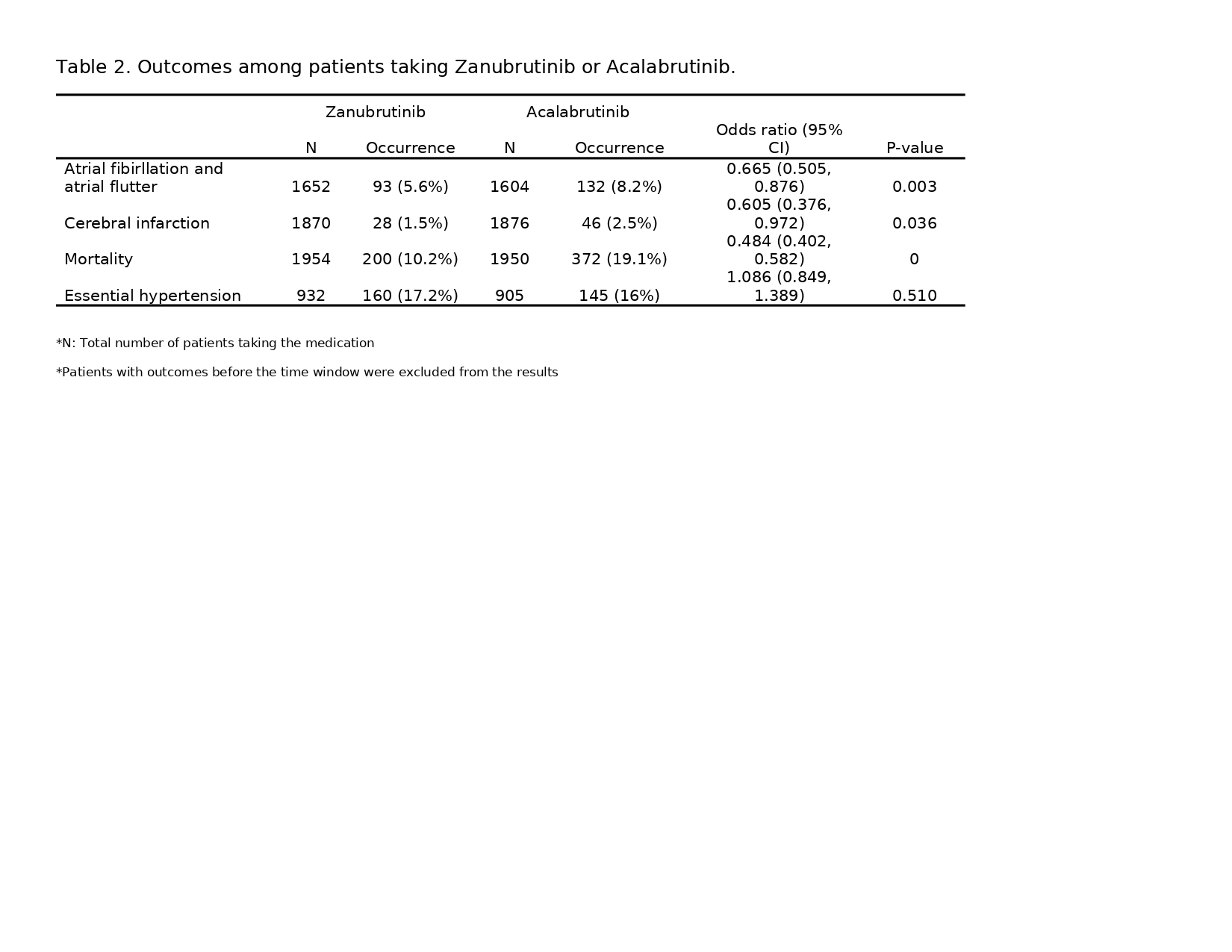
The incidence of atrial fibrillation/flutter was significantly lower in the zanubrutinib group
(5.70%) than in the acalabrutinib group (8.61%; OR 0.641, 95% CI 0.501–0.821; p = 0.0004),
though Kaplan-Meier analysis showed no difference in event-free survival (p = 0.286). Cerebral
infarction was also less common with zanubrutinib (1.42% vs. 2.23%; OR 0.631, 95% CI 0.404–
0.985; p = 0.0409), with no difference in event-free survival (p = 0.54). Hypertension rates were
similar (16.2% vs. 15.1%; OR 1.087, 95% CI 0.865–1.366; p = 0.47), though time-to-event
analysis favored acalabrutinib (p = 0.0009). All-cause mortality was significantly lower in the
zanubrutinib cohort (11.71% vs. 19.23%; OR 0.557, 95% CI 0.474–0.655; p < 0.0001), with
survival analysis confirming this finding (p = 0.001).
Conclusion:
In this large, real-world analysis, zanubrutinib was associated with lower rates of atrialfibrillation, cerebral infarction, and all-cause mortality compared to acalabrutinib. These findings
highlight potential cardiovascular safety advantages of zanubrutinib and support its consideration in patients at elevated cardiovascular risk. Prospective head-to-head trials are needed to confirm
these observations.
Next-generation Bruton’s tyrosine kinase inhibitors (BTKis) such as acalabrutinib and
zanubrutinib have improved treatment outcomes in B-cell malignancies including chronic
lymphocytic leukemia (CLL), mantle cell lymphoma (MCL), and Waldenström
macroglobulinemia (WM), while reducing off-target toxicities compared to ibrutinib. However,
their comparative cardiovascular safety profiles remain poorly characterized. This study
evaluates real-world cardiovascular and clinical outcomes between zanubrutinib and
acalabrutinib using a large multi-center database.
Methods:
We conducted a retrospective cohort study using the TriNetX Research Network (October 2017–
December 2024) including adult patients with CLL, MCL, WM, or small B-cell lymphoma
treated with zanubrutinib or acalabrutinib. Patients with prior exposure to other BTKis were
excluded. After 1:1 propensity score matching, 2,363 patients were included in each cohort. We
assessed 3-year outcomes: new-onset atrial fibrillation/flutter, cerebral infarction, hypertension,
and all-cause mortality using odds ratios (ORs), Kaplan-Meier survival analysis, and log-rank
testing.
Results:
The incidence of atrial fibrillation/flutter was significantly lower in the zanubrutinib group
(5.70%) than in the acalabrutinib group (8.61%; OR 0.641, 95% CI 0.501–0.821; p = 0.0004),
though Kaplan-Meier analysis showed no difference in event-free survival (p = 0.286). Cerebral
infarction was also less common with zanubrutinib (1.42% vs. 2.23%; OR 0.631, 95% CI 0.404–
0.985; p = 0.0409), with no difference in event-free survival (p = 0.54). Hypertension rates were
similar (16.2% vs. 15.1%; OR 1.087, 95% CI 0.865–1.366; p = 0.47), though time-to-event
analysis favored acalabrutinib (p = 0.0009). All-cause mortality was significantly lower in the
zanubrutinib cohort (11.71% vs. 19.23%; OR 0.557, 95% CI 0.474–0.655; p < 0.0001), with
survival analysis confirming this finding (p = 0.001).
Conclusion:
In this large, real-world analysis, zanubrutinib was associated with lower rates of atrialfibrillation, cerebral infarction, and all-cause mortality compared to acalabrutinib. These findings
highlight potential cardiovascular safety advantages of zanubrutinib and support its consideration in patients at elevated cardiovascular risk. Prospective head-to-head trials are needed to confirm
these observations.
More abstracts on this topic:
Anti-Arrhythmic drugs versus Catheter Ablation Prognostic value in the patients with Diastolic Heart Failure and Atrial Fibrillation: a Systematic Review and Meta-analysis of 38,237 Patients
Chichagi Fatemeh, Ghanbari Kimiya, Arbabi Mahta, Shirsalimi Niyousha, Sheikh Mahboobeh, Mohammadi Amirali, Alikhani Reyhaneh, Mombeini Hoda
A 50% or Greater Reduction in LDL-Cholesterol Is Associated with Improved Long-Term Outcomes and Lower Health Care Utilization After Myocardial Infarction - a SWEDEHEART studyReitan Christian, Watanabe Alexandre, Bash Lori, Galvain Thibaut, Arnet Urs, Jernberg Tomas