Final ID: MP1990
Impact of Functional Autoantibodies Against Endothelin-1 Receptor Type A and Angiotensin II Receptor Type 1 on Myocardial Dysfunction
Abstract Body (Do not enter title and authors here): Introduction: autoantibodies (AAs) activating endothelin-1 receptor type A (ETAR-AAs) and angiotensin II receptor type 1 (AT1R-AAs) are associated with microvascular obstruction, left ventricular remodeling and major adverse cardiovascular events after ST-elevation myocardial infarction (STEMI). Their association with myocardial dysfunction in the early phases after STEMI is still unknown.
Hypothesis: we hypothesized ETAR-AAs and AT1R-AAs, due to their proinflammatory and profibrotic effects, are associated with myocardial dysfunction in the early phases after STEMI.
Methods: we studied STEMI patients treated with primary PCI between February 2021 and April 2024 at Padua University Hospital. Blood samples for AAs level measurements were obtained within 12 h of admission. Patients were defined as seronegative or seropositive according to the AT1R-AA and ETAR-AA seropositivity threshold (>10 U/mL). Myocardial dysfunction was assessed measuring NTproBNP levels. NTproBNP levels were assessed routinely in all patients admitted for STEMI, either at admission or within 48 hours. NTproBNP levels were categorized as low/high according to the cutoff suggested for acute heart failure (300 pg/mL). We included in multivariable models measures of infarct extension and possible confounders (not including confounders which are not correlated with NTproBNP in our cohort).
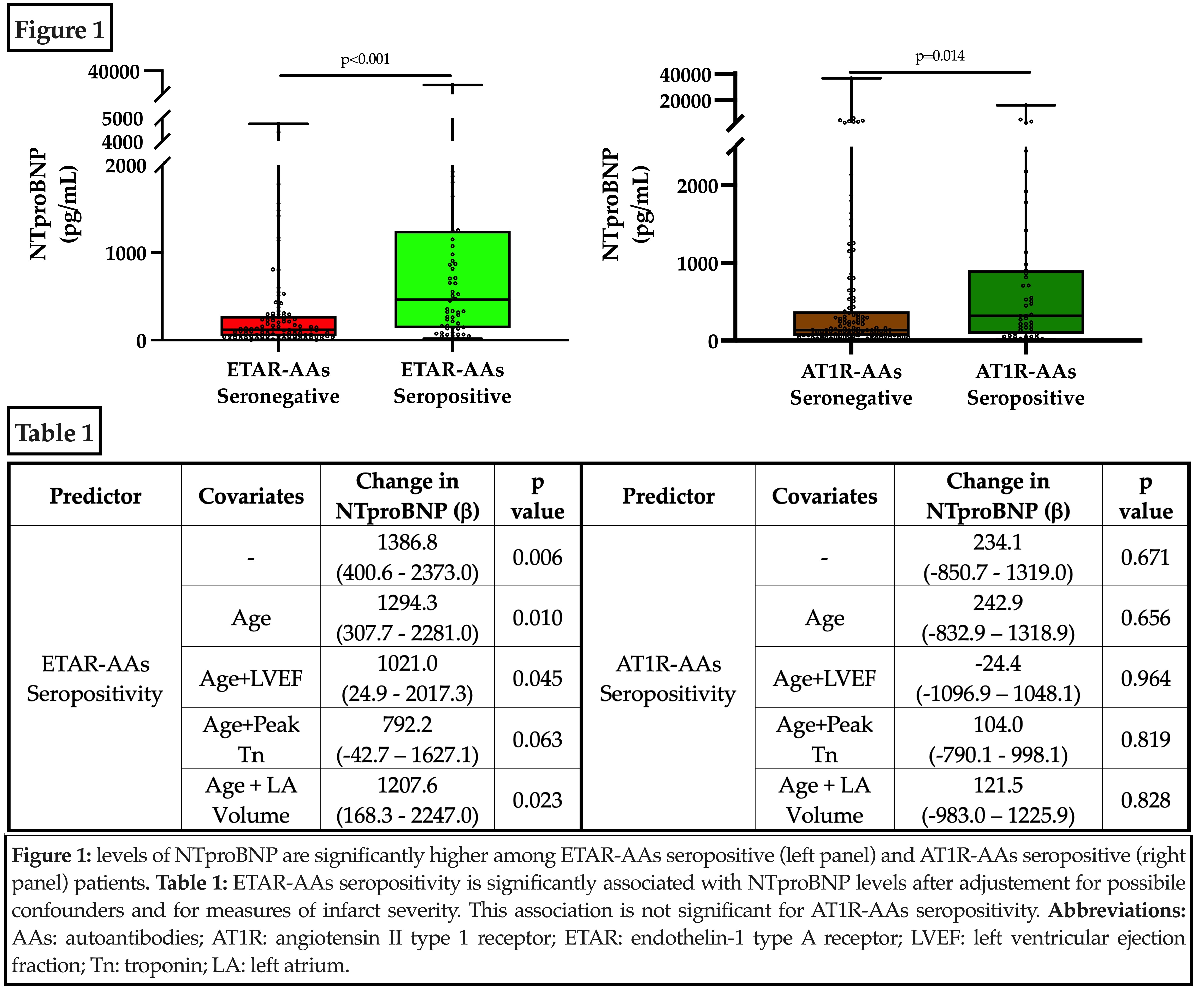
Results: 170 patients (median age 61 yrs, 82% males) were enrolled. Median NTproBNP was 163 pg/mL. NTproBNP was significantly correlated with ETAR-AAs (rho=0.253, p <0.001) and AT1R-AAs levels (rho=0.204, p=0.008). NTproBNP was significantly higher in ETAR-AAs seropositive (p<0.001) and in AT1R-AAs seropositive (p=0.014) patients compared to their seronegative counterparts (Figure 1). At multivariable linear regression, ETAR-AAs seropositivity was independently associated with NTproBNP levels, while AT1R-AAs seropositivity was not (Table 1). After multiple adjustment for all covariables reported in Table 1, ETAR-AAs positivity was associated with high NTproBNP levels (OR 5.0 (2.2-11.5), p<0.001).
Conclusions: ETAR-AAs are associated with myocardial dysfunction independently from features of STEMI severity and from most common confounders. These findings suggest that ETAR-AAs can induce myocardial dysfunction irrespectively of infarct extension, possibly through a direct effect on cardiomyocytes. Further studies in individuals without a recent acute coronary syndrome are warranted.
Hypothesis: we hypothesized ETAR-AAs and AT1R-AAs, due to their proinflammatory and profibrotic effects, are associated with myocardial dysfunction in the early phases after STEMI.
Methods: we studied STEMI patients treated with primary PCI between February 2021 and April 2024 at Padua University Hospital. Blood samples for AAs level measurements were obtained within 12 h of admission. Patients were defined as seronegative or seropositive according to the AT1R-AA and ETAR-AA seropositivity threshold (>10 U/mL). Myocardial dysfunction was assessed measuring NTproBNP levels. NTproBNP levels were assessed routinely in all patients admitted for STEMI, either at admission or within 48 hours. NTproBNP levels were categorized as low/high according to the cutoff suggested for acute heart failure (300 pg/mL). We included in multivariable models measures of infarct extension and possible confounders (not including confounders which are not correlated with NTproBNP in our cohort).
Results: 170 patients (median age 61 yrs, 82% males) were enrolled. Median NTproBNP was 163 pg/mL. NTproBNP was significantly correlated with ETAR-AAs (rho=0.253, p <0.001) and AT1R-AAs levels (rho=0.204, p=0.008). NTproBNP was significantly higher in ETAR-AAs seropositive (p<0.001) and in AT1R-AAs seropositive (p=0.014) patients compared to their seronegative counterparts (Figure 1). At multivariable linear regression, ETAR-AAs seropositivity was independently associated with NTproBNP levels, while AT1R-AAs seropositivity was not (Table 1). After multiple adjustment for all covariables reported in Table 1, ETAR-AAs positivity was associated with high NTproBNP levels (OR 5.0 (2.2-11.5), p<0.001).
Conclusions: ETAR-AAs are associated with myocardial dysfunction independently from features of STEMI severity and from most common confounders. These findings suggest that ETAR-AAs can induce myocardial dysfunction irrespectively of infarct extension, possibly through a direct effect on cardiomyocytes. Further studies in individuals without a recent acute coronary syndrome are warranted.
More abstracts on this topic:
An individual patient data meta-analysis of complete versus culprit-lesion only revascularization for acute myocardial infarction involving >8,800 individuals: The Complete Revascularization Trialists’ Collaboration
Mehta Shamir, Banning Amerjeet, Ramasundarahettige Chinthanie, Nguyen Helen, Wood David, Engstrom Thomas, Tiong Denise, Böhm Felix, James Stefan, Biscaglia Simone, Campo Gianluca, Smits Pieter, Giacoppo Daniele, Mccann Gerry
Ablation of Nephron Tubule Cell-Specific Npr1 Triggers High Blood Pressure and DysfunctionNeelamegam Kandasamy, Ramasamy Chandramohan, Pandey Kailash