Final ID: 4367184
Association of natriuretic peptide concentration with lifetime risk of heart failure in adults with diabetes mellitus: a pooled cohort analysis
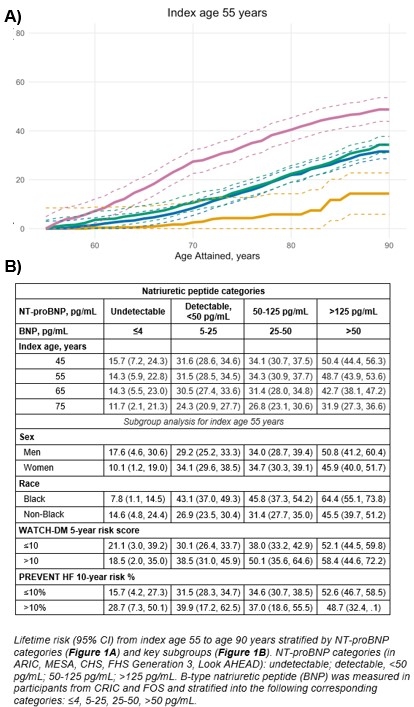
Methods: Participant-level data from 6 prospective cohorts (ARIC, MESA, CHS, FOS, FHS Generation 3, CRIC) and the Look AHEAD trial control group were pooled excluding participants with prevalent HF or ASCVD at baseline. Participants were stratified according to well-established NP thresholds (Figure). LTR of HF was determined at different index ages using the pratical incidence estimator macro with modified Kaplan-Meier methods that uses age as a time scale and mortality as a competing risk. A positive control group of adults with DM and prevalent CVD was analyzed separately.
Results: Among 5,986 participants (age 61 y, 45% male, 25% Black), 1,134 developed HF over 79,347 person-years (14.3 per 1,000 person-years). At index age 55 y, the LTR of HF through 90 years was 34.4%. Lifetime risk of HF increased progressively across increasing NT-proBNP categories at each index age (Figure 1A and 1B). At index age 55 y, the LTR estimate for the NT-proBNP >125 pg/mL category (48.7%) was comparable to the positive control group with prevalent CVD (n = 1,687; 51.7%). LTR of HF was higher in Black (vs. non-Black) adults at every category with detectable NT-proBNP and was comparable to prevalent CVD at lower thresholds (50-125 pg/ml) (Figure 1B). LTR of HF among adults with low short-term HF risk (based on WATCH-DM or 10-y HF PREVENT risk scores) and NT-proBNP >125 pg/mL was high and comparable with the prevalent CVD group. Adding NT-proBNP to 30-year PREVENT HF risk score substantially improved LTR prediction performance (AUROC for 30-year risk: 0.569 to 0.685, p<0.001).
Conclusions: In adults with DM, higher NT-proBNP concentrations identify higher LTR of HF, with the highest risk noted among those with concentrations >125 pg/ml supporting the current guideline recommended screening thresholds to discriminate lifetime risk. Lifetime risk of HF associated with NT-proBNP concentrations vary by race with disporporationtely high risk observed among Black adults.
- Segar, Matthew ( Texas Heart Institute , Houston , Texas , United States )
- Busui, Rodica ( UNIVERSITY MICHIGAN , Ann Arbor , Michigan , United States )
- Wilkins, John ( Northwestern University , Chicago , Illinois , United States )
- Espeland, Mark ( Wake Forest School of Medicine , Winston-Salem , North Carolina , United States )
- Bertoni, Alain ( WAKE FOREST UNIV SCHOOL MED , Pfafftown , North Carolina , United States )
- Bayes-genis, Antoni ( HUGTiP , Badalona , Spain )
- Pandey, Ambarish ( UT Southwestern Medical Center , Dallas , Texas , United States )
- Patel, Kershaw ( Houston Methodist Hospital , Houston , Texas , United States )
- De Lemos, James ( UT SOUTHWESTERN MEDICAL CTR , Dallas , Texas , United States )
- Vaduganathan, Muthiah ( Brigham and Womens Hospital , Boston , Massachusetts , United States )
- Ballantyne, Christie ( BAYLOR COLLEGE MEDICINE , Houston , Texas , United States )
- Defilippi, Chris ( University of maryland , Baltimore , Maryland , United States )
- Ayers, Colby ( UT Southwestern Medical Center , Dallas , Texas , United States )
- Januzzi, James ( Massachusetts General Hospital , Wellesley Hills , Massachusetts , United States )
- Dullaart, Robin ( University of Groningen , Groningen , Netherlands )
Meeting Info:
Session Info:
Novel Insights in CKM Prevalence and Risk Prediction
Monday, 11/10/2025 , 09:45AM - 11:00AM
Abstract Oral Session
More abstracts on this topic:
Sakboonyarat Boonsub, Poovieng Jaturon, Rangsin Ram
Acoramidis Lowers NT-proBNP in a Larger Proportion of ATTRibute-CM Study Participants With Transthyretin Amyloid Cardiomyopathy Compared with Placebo, Independent of Atrial Fibrillation StatusMaurer Mathew, Castano Adam, Tamby Jean-francois, Fox Jonathan, Mitter Sumeet, Hanna Mazen, Sperry Brett, Alexander Kevin, Obici Laura, Poulsen Steen, Januzzi James, Witteles Ronald, Jaber Wael, Brailovsky Yevgeniy, Vogtlaender Kai
More abstracts from these authors:
Chunawala Zainali, Garcia Katelyn, Wang Thomas, Bayes-genis Antoni, Pandey Ambarish, Patel Lajjaben, Keshvani Neil, Segar Matthew, Espeland Mark, Ballantyne Christie, Januzzi James, Lam Carolyn, Bertoni Alain
Intensive lifestyle intervention, cardiac biomarkers and atherosclerotic cardiovascular disease in type 2 diabetes and overweight or obesity – a post-hoc analysis of the Look Action for Health in Diabetes (AHEAD) trialPatel Kershaw, Bertoni Alain, Espeland Mark, Pandey Ambarish, Chunawala Zainali, Segar Matthew, Garcia Katelyn, Ndumele Chiadi, Wang Thomas, Januzzi James, Butler Javed, Lam Carolyn