Final ID: MP1398
ANCA-Negative Eosinophilic Myocarditis Masquerading as STEMI: A Case of Fulminant Cardiogenic Shock
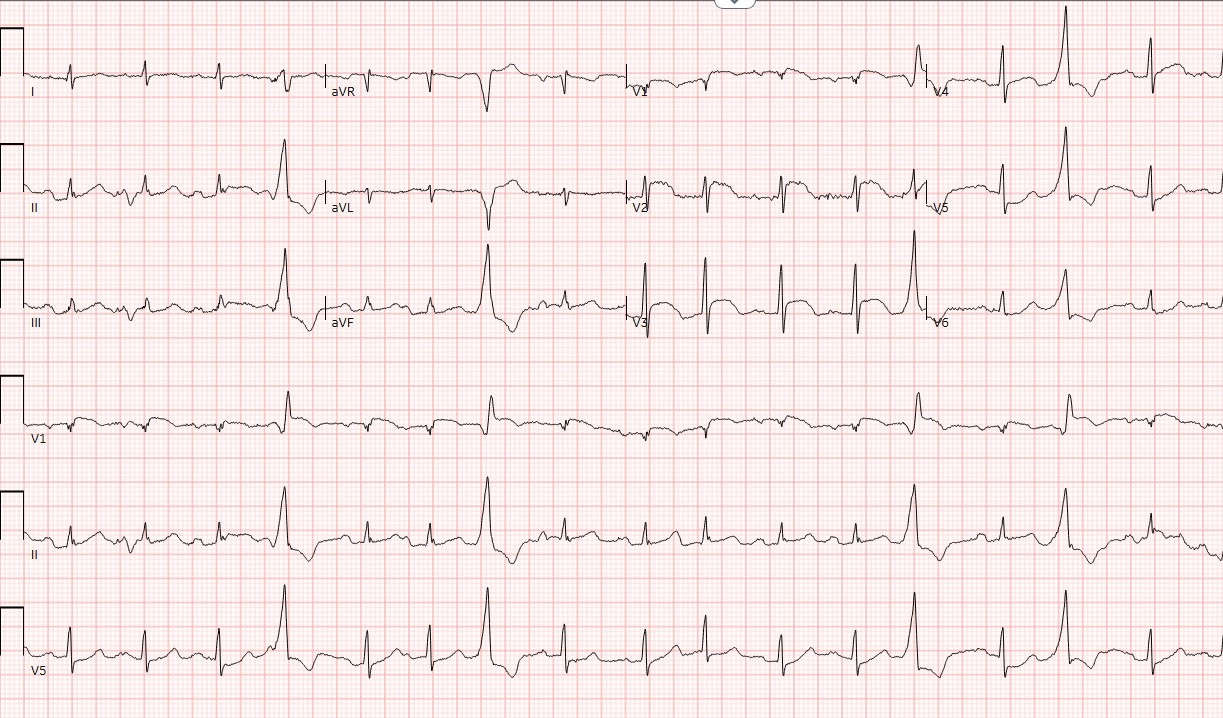
Abstract Body (Do not enter title and authors here): Description of case: A 79-year-old man with hypertension, diabetes, and mild asthma presented after three days of weakness, abdominal discomfort, and dyspnea without chest pain. Initial evaluation showed a troponin of 45,044 ng/L (normal < 14) and ST-elevations in V1–V5 with reciprocal depressions in II and III, prompting STEMI protocol activation. Emergent catheterization revealed nonobstructive coronary disease and an elevated left ventricular end-diastolic pressure of 28 mmHg. Echocardiography demonstrated severe left ventricular systolic dysfunction (EF 30 percent), mid-septal akinesis, and severe mitral regurgitation. Labs revealed relative eosinophilia with a normal absolute count, lymphopenia, and negative ANCA. Cardiac MRI showed heterogeneous mid-wall late gadolinium enhancement in the basal to mid-septum with elevated T1 and extracellular volume, suggesting nonischemic cardiomyopathy. After MRI, he developed fulminant cardiogenic shock with tachycardia, respiratory failure, and altered mental status requiring intubation, mechanical ventilation, norepinephrine, and vasopressin. Continuous venovenous hemofiltration was started for acute kidney injury. Endomyocardial biopsy confirmed eosinophilic myocarditis with extensive eosinophilic infiltration. Infectious workup—including blood cultures, respiratory viral panel, and serologies for Trichinella and Strongyloides—was negative. High-dose IV methylprednisolone (1 g daily) led to rapid improvement: extubation on day 5, vasopressor weaning, and transition to oral prednisone.
Discussion:This case illustrates the diagnostic challenge of ANCA-negative eosinophilic myocarditis presenting as STEMI. Massive troponin elevation and classic ST elevations suggested myocardial infarction with nonobstructive coronary arteries (MINOCA). Rapid deterioration and definitive biopsy revealed eosinophilic myocarditis. The absence of peripheral eosinophilia and negative ANCA delayed diagnosis, highlighting the necessity of endomyocardial biopsy in unexplained acute myocarditis with shock. Early recognition and prompt high-dose steroids are critical, as patients can deteriorate quickly but recover dramatically with treatment. Clinicians should suspect eosinophilic myocarditis in elderly patients with STEMI-like presentations and negative angiography, even if ANCA and absolute eosinophil counts are normal.
Discussion:This case illustrates the diagnostic challenge of ANCA-negative eosinophilic myocarditis presenting as STEMI. Massive troponin elevation and classic ST elevations suggested myocardial infarction with nonobstructive coronary arteries (MINOCA). Rapid deterioration and definitive biopsy revealed eosinophilic myocarditis. The absence of peripheral eosinophilia and negative ANCA delayed diagnosis, highlighting the necessity of endomyocardial biopsy in unexplained acute myocarditis with shock. Early recognition and prompt high-dose steroids are critical, as patients can deteriorate quickly but recover dramatically with treatment. Clinicians should suspect eosinophilic myocarditis in elderly patients with STEMI-like presentations and negative angiography, even if ANCA and absolute eosinophil counts are normal.
More abstracts on this topic:
A Case Presentation of Severe Left Ventricular Dysfunction from Focal Myocarditis due to Immune Checkpoint Inhibitor
Patel Romil, Hussain Kifah, Gordon Robert
A Heart Transplant Patient’s Mysterious Illness: A Diagnostic OdysseyAlkalbani Mutaz, Nayer Hassan, Cochrane Adam, Saeed Ibrahim, Psotka Mitchell, Rollins Allman, Kennedy Jamie, Blumer Vanessa