Final ID: Mo2014
Low Rates Of Escalation Of Lipid Lowering Therapy Amongst Atherosclerotic Cardiovascular Disease Patients With Uncontrolled LDL-C
Abstract Body (Do not enter title and authors here): Background: In patients with atherosclerotic cardiovascular disease (ASCVD), guidelines recommend a reduction in low-density lipoprotein cholesterol (LDL-C) to target levels with statin therapy as required. Where targets are not achieved, escalation to higher intensity statin +/- additional lipid-lowering therapy (LLT) is recommended. It is unknown to what extent adjustments in LLT are made after LLT initiation in routine practice, in relation to measured LDL-C levels.
Aims: To document (i) testing and (ii) achievement of ESC guideline-recommended LDL-C levels (<1.8 mmol/L), in relation to (iii) prescribed LLT regimen during the first two years post-ASCVD diagnosis.
Methods: A retrospective, population-level, observational study using linked anonymised population electronic health record (EHR) data amongst 178696 patients diagnosed with ASCVD between 2010-22, with at least one year of follow-up data. Patients were followed up for two years post-diagnosis, and censored at the point of death, migration, or loss of linked primary care data.
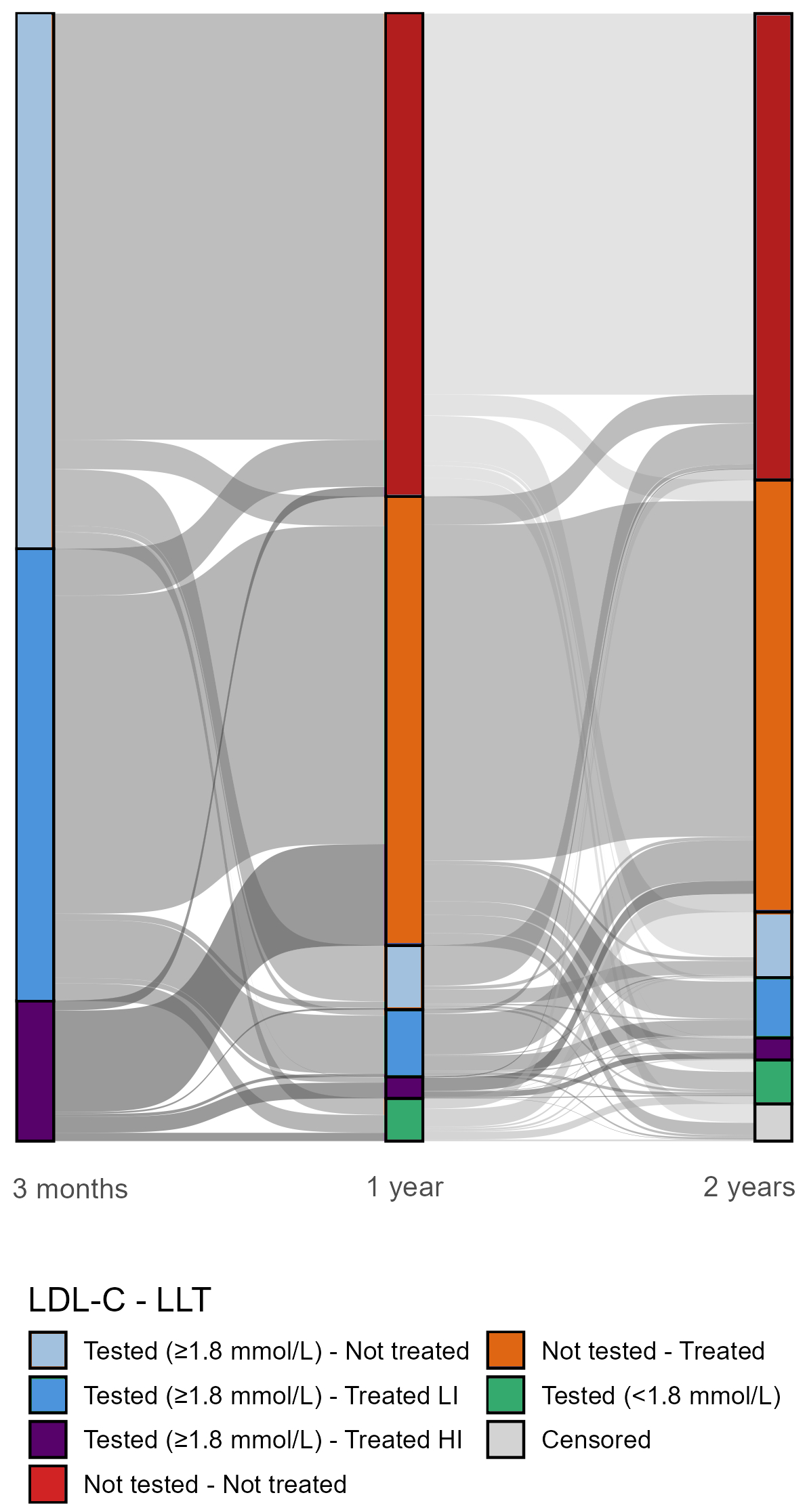
Results: Within 90-days post-diagnosis only 36318 (20.3%) patients had LDL-C levels documented in their EHR, of which 7.3% were <1.8 mmol/L. Of those 23446 (13.1%) patients with LDL-C ≥1.8 mmol/L, 12.7% were receiving high-intensity statin therapy or combination LLT (HI), 40% had lower-intensity statin therapy or other LLT monotherapy (LI) and 47.3% were not treated (Figure 1). During the first-year post-diagnosis, only 4222 (2.4%) had LDL-C tested and 929 (22%) of these achieved target. Of those not achieving target, 15.9% were prescribed HI-LLT, 43.4% LI-LLT, and 40.7% were not treated (Figure 1). Among patients with no test at one-year, 48.1% were prescribed LLT and 51.9% were not treated. Of those not treated, 78.7% received no test or treatment by two-years post-diagnosis. By two-years post-ASCVD diagnosis, 12.5%, 27.2%, and 54.5% were prescribed HI, LI, and no LLT respectively. Figure 1 illustrates that most patients were not tested following 90-days post-diagnosis and remained on the initial LLT regime over the subsequent two-years.
Conclusions: Management of lipids was below guideline-recommended standards in the early years following ASCVD diagnosis in the population, with low levels of testing and escalation in lipid treatment regimen uncommon, even when indicated by documented LDL-C levels. A more rigorous system-wide approach to LLT is required to maximise the potential benefits among these very high-risk patients.
Aims: To document (i) testing and (ii) achievement of ESC guideline-recommended LDL-C levels (<1.8 mmol/L), in relation to (iii) prescribed LLT regimen during the first two years post-ASCVD diagnosis.
Methods: A retrospective, population-level, observational study using linked anonymised population electronic health record (EHR) data amongst 178696 patients diagnosed with ASCVD between 2010-22, with at least one year of follow-up data. Patients were followed up for two years post-diagnosis, and censored at the point of death, migration, or loss of linked primary care data.
Results: Within 90-days post-diagnosis only 36318 (20.3%) patients had LDL-C levels documented in their EHR, of which 7.3% were <1.8 mmol/L. Of those 23446 (13.1%) patients with LDL-C ≥1.8 mmol/L, 12.7% were receiving high-intensity statin therapy or combination LLT (HI), 40% had lower-intensity statin therapy or other LLT monotherapy (LI) and 47.3% were not treated (Figure 1). During the first-year post-diagnosis, only 4222 (2.4%) had LDL-C tested and 929 (22%) of these achieved target. Of those not achieving target, 15.9% were prescribed HI-LLT, 43.4% LI-LLT, and 40.7% were not treated (Figure 1). Among patients with no test at one-year, 48.1% were prescribed LLT and 51.9% were not treated. Of those not treated, 78.7% received no test or treatment by two-years post-diagnosis. By two-years post-ASCVD diagnosis, 12.5%, 27.2%, and 54.5% were prescribed HI, LI, and no LLT respectively. Figure 1 illustrates that most patients were not tested following 90-days post-diagnosis and remained on the initial LLT regime over the subsequent two-years.
Conclusions: Management of lipids was below guideline-recommended standards in the early years following ASCVD diagnosis in the population, with low levels of testing and escalation in lipid treatment regimen uncommon, even when indicated by documented LDL-C levels. A more rigorous system-wide approach to LLT is required to maximise the potential benefits among these very high-risk patients.
More abstracts on this topic:
A Health Coach-Based Multi-Level Personalized Strategy Lowers LDL-Cholesterol and Enhances Lipid Control in Veterans with Atherosclerotic Cardiovascular Disease – The VA Lipid Optimization Reimagined Quality Improvement Project at VA New York Harbor Healthcare System
Chen Tina, Ingerman Diana, Haley Leah, Salovaara Priscilla, Nicholson Andrew, Illenberger Nicholas, Natarajan Sundar
Comparative Study of Coronary Artery Disease (CAD) Prediction: Conventional QRISK3 vs. Enhanced Machine Learning Models Combined with Particle Swarm Optimization (PSO) AlgorithmHarmadha Wigaviola Socha Purnamaasri, Wang Dennis, Masood Mohsin