Final ID: 4365796
Cumulative Life-course Blood Pressure Burden and Steepness of Increase Are Associated with Reduced Myocardial Perfusion in Older Age: Insights from MyoFit46
Aim: We explored the impact of life-course BP, especially the steepness of BP increase and cumulative BP burden, on later-life stress myocardial blood flow (sMBF) and perfusion reserve (MPR) by cardiovascular magnetic resonance (CMR).
Methods: MyoFit46 prospectively undertook stress perfusion and late gadolinium enhancement (LGE) CMR at age 76 in age-matched participants of the National Survey of Health and Development 1946 birth cohort. Myocardial perfusion was quantified as global sMBF normalized (sMBFN) to contemporaneous rate pressure product (heart rate x central aortic BP) and MPR. Systolic (SBPs) and diastolic BPs (DBPs) were recorded at 36, 43, 53, 62, 69, and 76 years. For each participant, annual rates of BP change (steepness) and the area under the BP trajectory curve (AUCBP; cumulative burden) were calculated using mixed-effect models. Participants were clustered by BP trajectory using latent class mixed models. Associations between BP and CMR metrics were tested using generalized models, adjusted for antihypertensive use, demographics, lifestyle, and comorbidities. Mediation analyses explored mechanistic pathways.
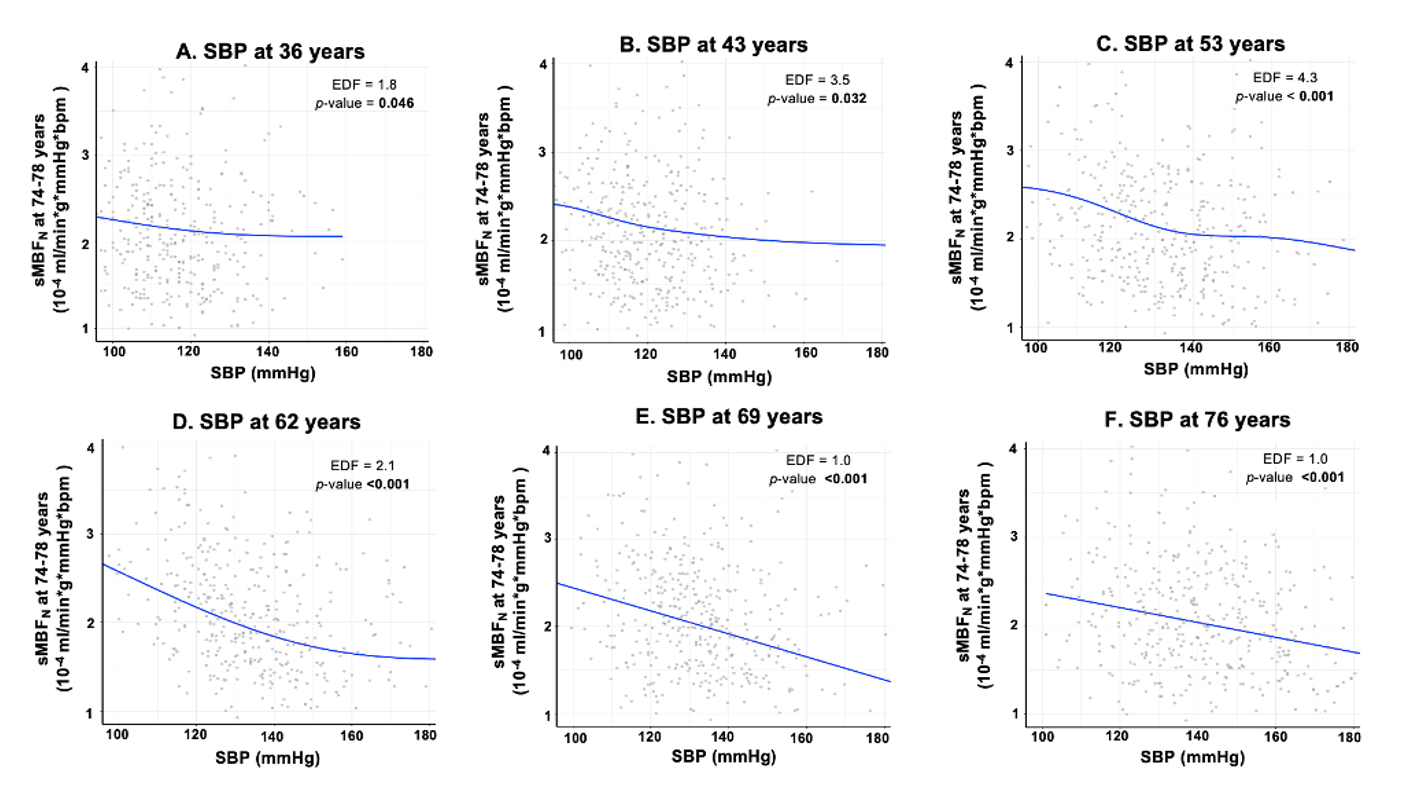
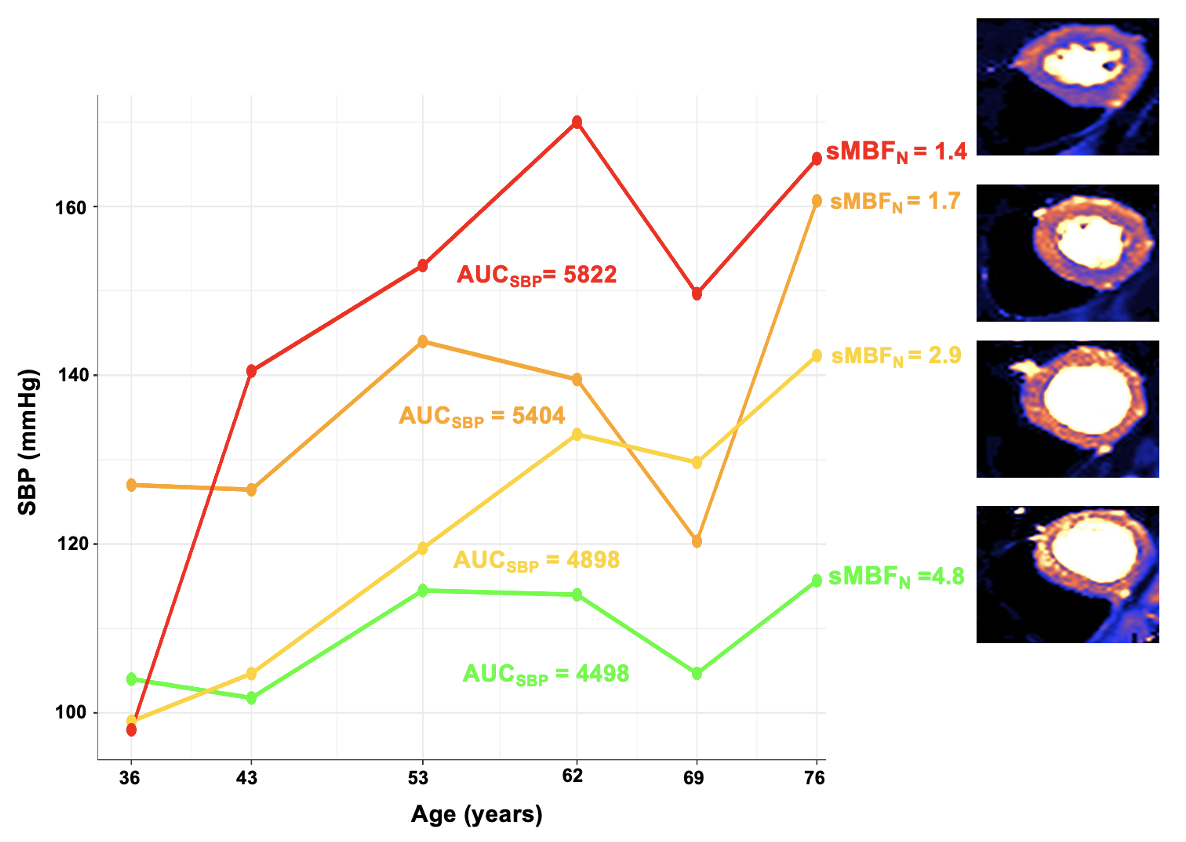
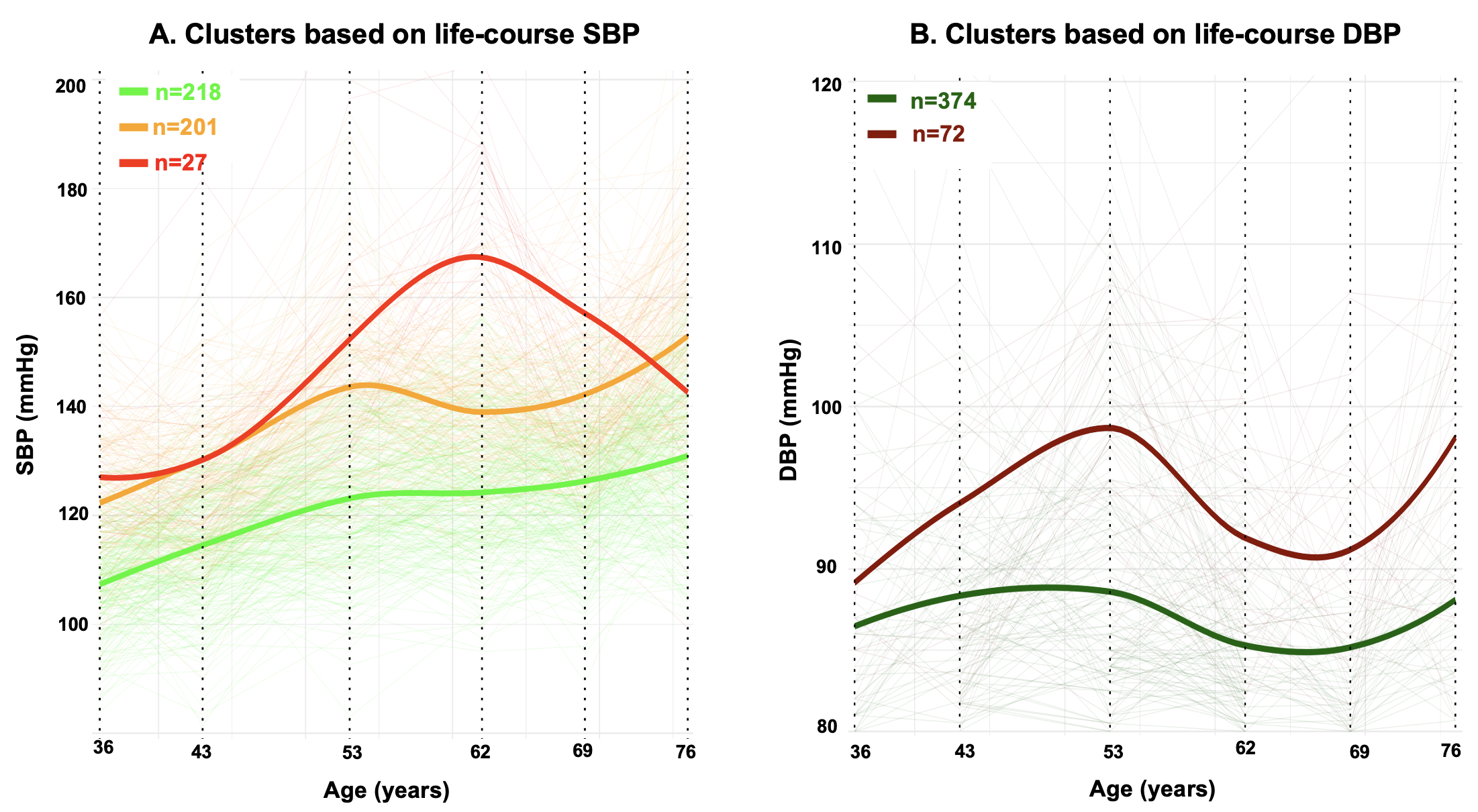
Results: Among 459 participants (53% male), each 10mmHg SBP increase at 36, 43, 53, 62, and 69 years associated with a 3-6% lower sMBFN at 76. For midlife BPs (43-62 years), associations were independent of SBP at 76 and the decrease in sMBFN was steepest as SBPs rose from 120 to 140mmHg (Figure 1). Having a sustained higher SBP by 10mmHg from 36 to 76 years associated with an 11% (95% CI: 8-14) lower sMBFN. Exemplar CMR perfusion maps based on AUCSBP are shown in Figure 2. Each 1 mmHg/year steeper SBP rise during age intervals 36–43, 43–53, 53–62, and 62–69 was associated with a 2–5% lower sMBFN at age 76, independent of baseline or final BPs in each interval. sMBFN mediated 20-40% of the life-course SBPs and myocardial fibrosis by LGE associations. Results were similar for DBP, MPR, or unnormalized sMBF. Participants with the steepest BP rises from 36 to 53 years had the lowest myocardial perfusion at 76 (Figure 3).
Conclusion: Higher life-course BPs (even from age 36), steeper increases (regardless of final BP), and more years spent at higher BP levels associate with lower myocardial perfusion in older age. This underscores the importance of early-life BP screening, guiding treatment based on BP trajectories and cumulative burden, and rigorous midlife BP control.
- Topriceanu, Constantin-cristian ( University College London , London , United Kingdom )
- Wong, Andrew ( University College London , London , United Kingdom )
- Pierce, Iain ( Barts Heart Centre , London , United Kingdom )
- Davies, Rhodri ( University College London , London , United Kingdom )
- Lambiase, Pier ( Barts Heart Centre , London , United Kingdom )
- Chaturvedi, Nishi ( University College London , London , United Kingdom )
- Kellman, Peter ( National Institute of Health , Bethesda , Maryland , United States )
- Hardy, Rebecca ( Loughborough University , Loughborough , United Kingdom )
- Moon, James ( Barts Heart Centre , London , United Kingdom )
- Hughes, Alun ( University College London , London , United Kingdom )
- Captur, Gabriella ( University College London , London , United Kingdom )
- Webber, Matthew ( University College London , London , United Kingdom )
- Shiwani, Hunain ( University College London , London , United Kingdom )
- Chan, Fiona ( University College London , London , United Kingdom )
- Martin, Emma ( University College London , London , United Kingdom )
- Falconer, Debbie ( University College London , London , United Kingdom )
- Bennett, Jonathan ( University College London , London , United Kingdom )
- Gonzalez Martin, Pablo ( University College London , London , United Kingdom )
- Shah, Haytham ( University College London , London , United Kingdom )
Meeting Info:
Session Info:
Melvin Judkins Early Career Clinical Investigator Award Competition
Saturday, 11/08/2025 , 09:45AM - 11:00AM
Abstract Oral Session
More abstracts on this topic:
Pardee Lisa, Bochicchio Lauren, Caceres Billy
A Case of Caseous Mitral Annular Calcification and the Utility of Multimodality Cardiac ImagingNguyen Amanda, English Carter, Ghasemiesfe Ahmadreza, Venugopal Sandhya
More abstracts from these authors:
Joy George, Davies Rhodri, Meredith Benjamin, Pierce Iain, Shiwani Hunain, Kellman Peter, Treibel Thomas, Manisty Charlotte, Hughes Alun, Moon James
Diagnostic 12-lead ECGs at Rest and during Stress in a 3T MR Scanner: A Novel System for In-bore Cardiac Monitoring and Ischemia DetectionFalconer Debbie, Moon James, Hughes Alun, Odille Freddy, Calmon Guillaume, Captur Gabriella, Mehri Maroua, Bhiri Mohammed, Webber Matthew, Whitmore Isabelle, Martin Emma, Vagliani Giovanni, Kellman Peter, Lambiase Pier