Final ID: MP1501
Therapeutic Gaps in Lipid Management Among Patients with Prior ASCVD Hospitalized with Acute Myocardial Infarction: Insights from the NCDR Chest Pain-MI Registry
Abstract Body (Do not enter title and authors here): Background: Lipid-lowering therapy (LLT) is essential for secondary prevention in patients with atherosclerotic cardiovascular disease (ASCVD). However, real-world data on LLT use, lipid control, and treatment intensification in patients with prior ASCVD who are newly hospitalized with acute myocardial infarction (AMI) are limited. In this nationwide study, we assessed the quality of lipid management for ASCVD patients hospitalized with a new AMI in the U.S.
Methods: We evaluated patients with pre-existing ASCVD who were hospitalized with AMI in the NCDR Chest Pain–MI Registry between January 2019 and March 2023. Primary outcomes were outpatient LLT prescription on admission and LDL-C levels checked during or within 6 months prior to hospitalization. Using discharge medication data which were only available after 2020, we also evaluated the proportion of patients discharged on combination LLT (≥2 agents) as a secondary outcome. Variables were compared using Wilcoxon rank-sum tests and chi-square tests as appropriate.
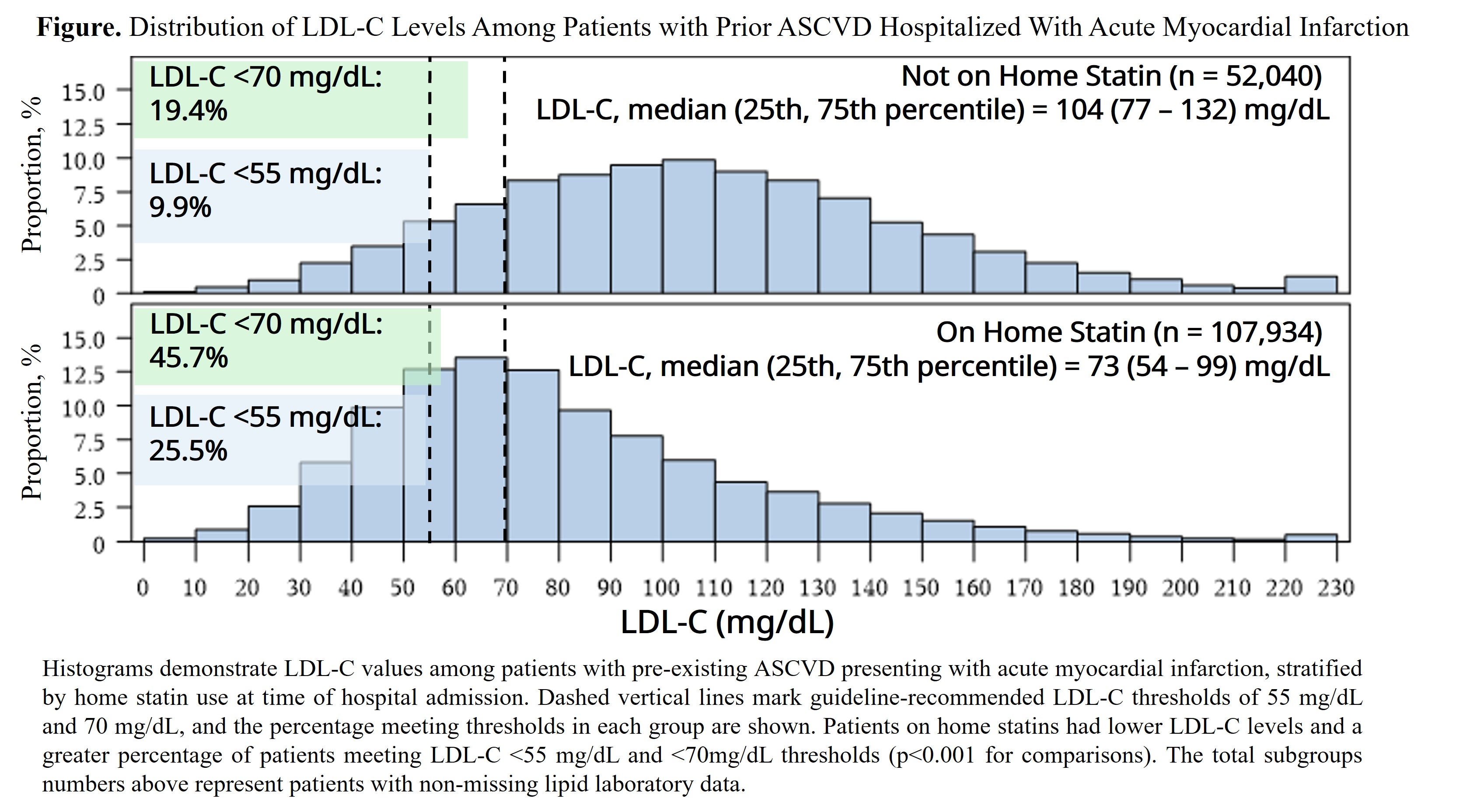
Results: The study cohort included 217,812 patients with pre-existing ASCVD admitted with AMI at 677 hospitals. The median (25th, 75th percentile) age was 69 years (60–77), and 31.9% were women. Prior to admission, 31.5% were not prescribed a statin, and only 3.7% were prescribed combination LLT. The median (25th, 75th percentile) serum LDL-C was 81 mg/dL (59–112), including 73 mg/dL (54–99) for statin users vs. 104 mg/dL (77–132) for non-statin users (p<0.001). Among all patients with data available, 20.4% had LDL-C <55 mg/dL and 37.1% had LDL-C<70 mg/dL. Patients previously taking statins were significantly more likely to have lower LDL-C and meet guideline-recommended goals upon admission (Figure). Among patients with discharge data available, 93.3% were discharged on a statin, 88.9% on a high-intensity statin, and 1.7% on a PCSK9 inhibitor. Only 10.4% of patients were discharged with combination LLT. The median (25th, 75th percentile) percentage of patients discharged on combination LLT across hospitals was 9.0% (5.7-13.0%).
Conclusions: Despite having established ASCVD before AMI admission, nearly 1 in 3 patients were not on a statin and only 1 in 5 had appropriate LDL-C levels based on guidelines. Only one in ten patients was prescribed combination LLT at discharge. These findings reflect missed opportunities for secondary prevention and emphasize the need for more aggressive lipid management in the outpatient and inpatient settings.
Methods: We evaluated patients with pre-existing ASCVD who were hospitalized with AMI in the NCDR Chest Pain–MI Registry between January 2019 and March 2023. Primary outcomes were outpatient LLT prescription on admission and LDL-C levels checked during or within 6 months prior to hospitalization. Using discharge medication data which were only available after 2020, we also evaluated the proportion of patients discharged on combination LLT (≥2 agents) as a secondary outcome. Variables were compared using Wilcoxon rank-sum tests and chi-square tests as appropriate.
Results: The study cohort included 217,812 patients with pre-existing ASCVD admitted with AMI at 677 hospitals. The median (25th, 75th percentile) age was 69 years (60–77), and 31.9% were women. Prior to admission, 31.5% were not prescribed a statin, and only 3.7% were prescribed combination LLT. The median (25th, 75th percentile) serum LDL-C was 81 mg/dL (59–112), including 73 mg/dL (54–99) for statin users vs. 104 mg/dL (77–132) for non-statin users (p<0.001). Among all patients with data available, 20.4% had LDL-C <55 mg/dL and 37.1% had LDL-C<70 mg/dL. Patients previously taking statins were significantly more likely to have lower LDL-C and meet guideline-recommended goals upon admission (Figure). Among patients with discharge data available, 93.3% were discharged on a statin, 88.9% on a high-intensity statin, and 1.7% on a PCSK9 inhibitor. Only 10.4% of patients were discharged with combination LLT. The median (25th, 75th percentile) percentage of patients discharged on combination LLT across hospitals was 9.0% (5.7-13.0%).
Conclusions: Despite having established ASCVD before AMI admission, nearly 1 in 3 patients were not on a statin and only 1 in 5 had appropriate LDL-C levels based on guidelines. Only one in ten patients was prescribed combination LLT at discharge. These findings reflect missed opportunities for secondary prevention and emphasize the need for more aggressive lipid management in the outpatient and inpatient settings.
More abstracts on this topic:
A Community-Based Intervention to Improve Cardiovascular Health Understanding in the Dallas-Fort Worth South Asian Community
Deo Parminder, Rohatgi Anand, Sharma Parul, Sathyamoorthy Mohanakrishnan
A Multimodal Artificial Intelligence Signature of Advanced Cardiac and Vascular Aging Defines Elevated Risk of Cardiovascular DiseasePerera Sudheesha, Biswas Dhruva, Dhingra Lovedeep, Aminorroaya Arya, Coppi Andreas, Khera Rohan