Final ID: Su3147
Access to Lipid-Lowering Therapies is Limited by Payer Coverage Restrictions and High Out-of-Pocket Costs on Medicare Prescription Drug Plans
Abstract Body (Do not enter title and authors here): Introduction/Background: There is an urgent need to improve lipid control as one in four adults in the United States has elevated low-density lipoprotein cholesterol (LDL-C). Many non-statin lipid-lowering therapies such as ezetimibe, pro-protein convertase subtilisin-kexin type 9 inhibitors (PCSK9i), bempedoic acid, and icosapent ethyl are recommended for LDL-C and cardiovascular risk reduction, but usage remains suboptimal. Proposed barriers include payer restrictions and patient costs, but the extent of these issues for Medicare beneficiaries in the contemporary period is poorly defined.
Research Questions/Hypotheses: To what extent do Medicare Prescription Drug Plans provide coverage or use payer management strategies to restrict access to lipid-lowering medications? What are the patient out-of-pocket expenses for these therapies?
Methods/Approach: Plan coverage, payer restrictions, and annual out-of-pocket costs were extracted from Medicare Prescription Drug Plan files from July-September 2023. Medications studied included generic atorvastatin, rosuvastatin, and ezetimibe as well as brand-name PCSK9i, bempedoic acid, and icosapent ethyl.
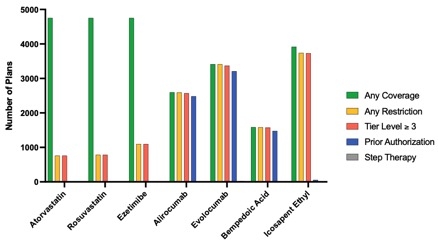
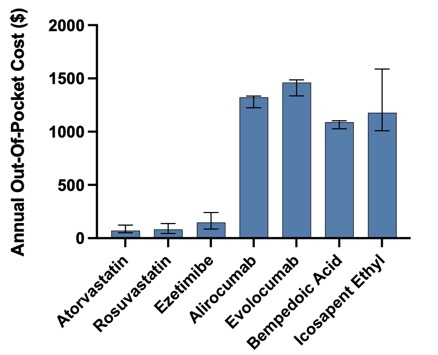
Results/Data: Among 4,754 plans, coverage of lipid-lowering therapies varied widely. Generic atorvastatin, rosuvastatin, and ezetimibe were universally covered, while branded therapies such as alirocumab and bempedoic acid were covered by only one-half and one-third of plans, respectively. Nearly all plans providing coverage placed non-generic medications in high cost-sharing tiers and required prior authorization for alirocumab (96% of plans), evolocumab (94% of plans), and bempedoic acid (93% of plans). Median annual out-of-pocket costs ranged from $71 to $147 for generic statins and ezetimibe, while patient expenses for all branded lipid-lowering therapies exceeded $1,000.
Conclusions: Lack of coverage, widespread prior authorization requirements, and high out-of-pocket costs jeopardize access to non-generic lipid-lowering medications, and likely contribute to their low utilization in the mitigation of cardiovascular disease risk. Some cost toxicity for patients may be alleviated by the Inflation Reduction Act and additional Medicare negotiations on drug pricing, however addressing the barriers of limited coverage and payer restrictions will be paramount to improve use of these therapies.
Research Questions/Hypotheses: To what extent do Medicare Prescription Drug Plans provide coverage or use payer management strategies to restrict access to lipid-lowering medications? What are the patient out-of-pocket expenses for these therapies?
Methods/Approach: Plan coverage, payer restrictions, and annual out-of-pocket costs were extracted from Medicare Prescription Drug Plan files from July-September 2023. Medications studied included generic atorvastatin, rosuvastatin, and ezetimibe as well as brand-name PCSK9i, bempedoic acid, and icosapent ethyl.
Results/Data: Among 4,754 plans, coverage of lipid-lowering therapies varied widely. Generic atorvastatin, rosuvastatin, and ezetimibe were universally covered, while branded therapies such as alirocumab and bempedoic acid were covered by only one-half and one-third of plans, respectively. Nearly all plans providing coverage placed non-generic medications in high cost-sharing tiers and required prior authorization for alirocumab (96% of plans), evolocumab (94% of plans), and bempedoic acid (93% of plans). Median annual out-of-pocket costs ranged from $71 to $147 for generic statins and ezetimibe, while patient expenses for all branded lipid-lowering therapies exceeded $1,000.
Conclusions: Lack of coverage, widespread prior authorization requirements, and high out-of-pocket costs jeopardize access to non-generic lipid-lowering medications, and likely contribute to their low utilization in the mitigation of cardiovascular disease risk. Some cost toxicity for patients may be alleviated by the Inflation Reduction Act and additional Medicare negotiations on drug pricing, however addressing the barriers of limited coverage and payer restrictions will be paramount to improve use of these therapies.
More abstracts on this topic:
A multifaceted family intervention for blood pressure management in rural China: an open label, parallel group, cluster randomized trial (Healthy Family Program)
A blood test based on RNA-seq and machine learning for the detection of steatotic liver disease: A Pilot Study on Cardiometabolic Health
Jiang Chao, Dong Jianzeng, Cai Jun, Anderson Craig, Du Xin, Tang Yangyang, Han Rong, Song Yanna, Wang Chi, Lin Xiaolei, Yi Yang, Rodgers Anthony, Ma Changsheng
A blood test based on RNA-seq and machine learning for the detection of steatotic liver disease: A Pilot Study on Cardiometabolic Health
Poggio Rosana, Berdiñas Ignacio, La Greca Alejandro, Luzzani Carlos, Miriuka Santiago, Rodriguez-granillo Gaston, De Lillo Florencia, Rubilar Bibiana, Hijazi Razan, Solari Claudia, Rodríguez Varela María Soledad, Mobbs Alan, Manchini Estefania