Final ID: Sa3084
Outcomes of Heart Failure in Muscular Dystrophies in Adults: A Nationwide Analysis in the United States
Abstract Body (Do not enter title and authors here): Background: Muscular dystrophies (MDs) may cause heart failure (HF), but outcomes specific to MD-related HF are not well characterized.
Research Question: Do the outcomes of HF hospitalizations differ between patients with underlying MDs (MD-HF) vs. patients without MDs (non-MD-HF) in the United States?
Methods: Discharge data from HF hospitalizations were abstracted from the Nationwide Readmissions Database (2016-2022) and stratified by the presence or absence of MD (MD-HF vs. non-MD-HF). Logistic regression and lognormal models were estimated to assess differences in inpatient mortality, length of stay (LOS), total costs, complications, and 30-day and 90-day all-cause readmissions. Propensity-score matching (PSM) was used to control baseline differences between the MD-HF and non-MD-HF cohorts. Odds ratios (OR) with associated 95% Confidence intervals (CI) and p-values were reported. Analyses were conducted via SAS v. 9.4, with statistical significance indicated by two-tailed p<.05.
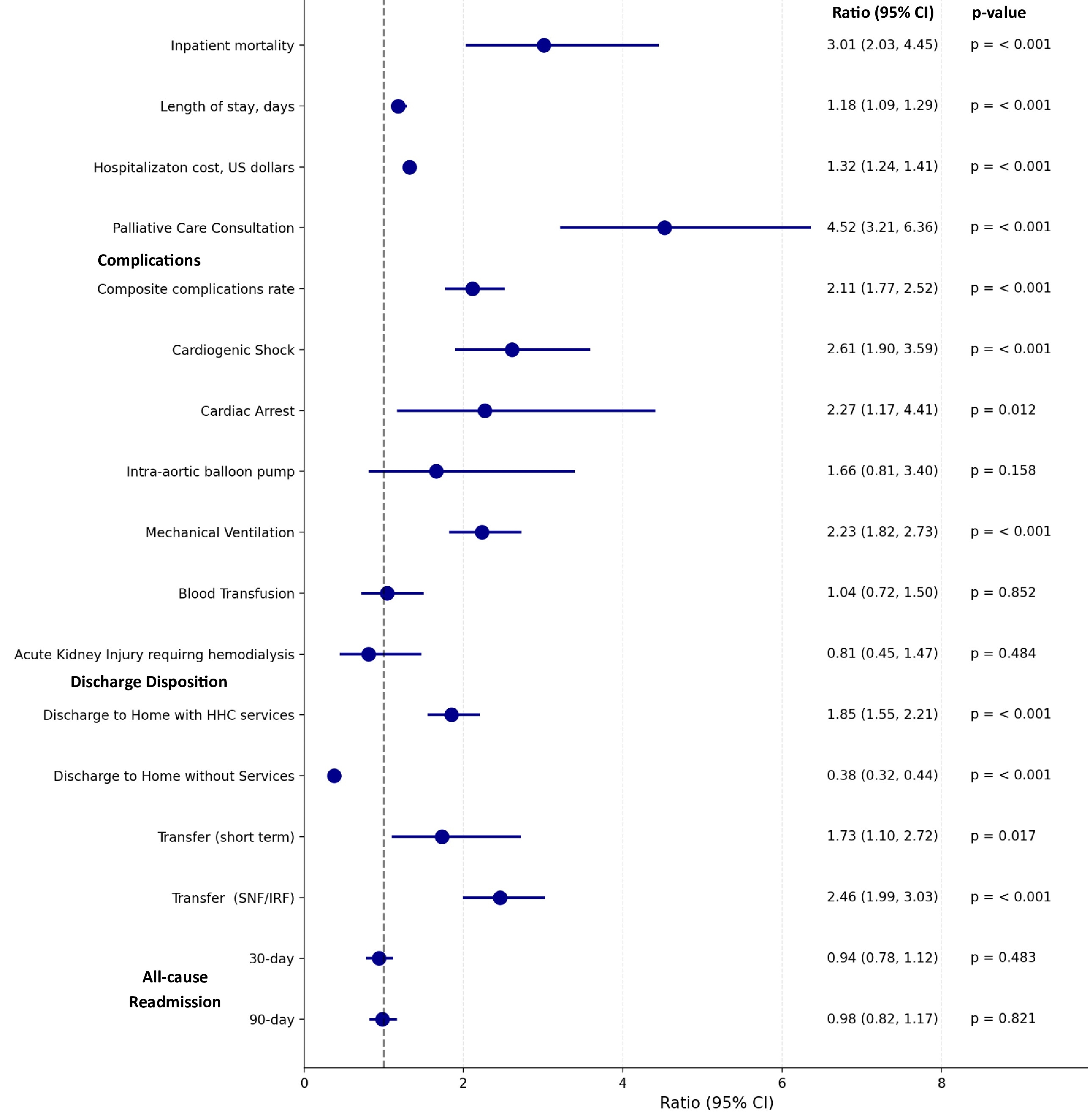
Results: 8,466,806 HF hospitalizations were included in the analysis, of which 3688 (0.04%) involved patients with MD. MD-HF hospitalizations involved younger patients (mean age 55.3 vs. 71.3 years, p<0.001) with higher rates of HF with reduced ejection fraction (HFrEF) compared to non-MD-HF hospitalizations (48.1% vs. 34.9%, p<0.001). Compared to non-MD-HF hospitalizations (2.01%), MD-HF hospitalizations (5.82%) were associated with significantly higher odds of inpatient mortality (OR 3.01, 95% CI: 2.03, 4.45); higher complications rate (OR 2.11, 95% CI, 1.77, 2.52) including cardiogenic shock (OR 2.61, 95% CI, 1.90, 3.59), cardiac arrest (OR 2.27, 95% CI, 1.17, 4.41), use of mechanical ventilation (OR 2.23, 95% CI, 1.82, 2.73); higher palliative care consultation (OR 4.52, 95% CI, 3.21, 6.36); as well as more extended hospital LOS (OR 1.18, 95% CI, 1.09, 1.29), higher total costs (OR 1.32, 95% CI, 1.24, 1.41), and higher odds of discharge to rehab facility (OR 2.46, 95% CI, 1.99, 3.03) and home healthcare (OR 1.85, 95% CI, 1.55, 2.21) (all p<0.001). MD was not associated with a significant difference in 30-day (OR 0.94, 95% CI, 0.78, 1.12) and 90-day (OR 0.98, 95% CI, 0.82, 1.17) all-cause readmission rates.
Conclusion: MD-HF hospitalizations were associated with higher inpatient mortality, complication rates, resource utilization, discharge to rehab facility and home healthcare, and no difference in readmission rates compared to non-MD-HF hospitalizations.
Research Question: Do the outcomes of HF hospitalizations differ between patients with underlying MDs (MD-HF) vs. patients without MDs (non-MD-HF) in the United States?
Methods: Discharge data from HF hospitalizations were abstracted from the Nationwide Readmissions Database (2016-2022) and stratified by the presence or absence of MD (MD-HF vs. non-MD-HF). Logistic regression and lognormal models were estimated to assess differences in inpatient mortality, length of stay (LOS), total costs, complications, and 30-day and 90-day all-cause readmissions. Propensity-score matching (PSM) was used to control baseline differences between the MD-HF and non-MD-HF cohorts. Odds ratios (OR) with associated 95% Confidence intervals (CI) and p-values were reported. Analyses were conducted via SAS v. 9.4, with statistical significance indicated by two-tailed p<.05.
Results: 8,466,806 HF hospitalizations were included in the analysis, of which 3688 (0.04%) involved patients with MD. MD-HF hospitalizations involved younger patients (mean age 55.3 vs. 71.3 years, p<0.001) with higher rates of HF with reduced ejection fraction (HFrEF) compared to non-MD-HF hospitalizations (48.1% vs. 34.9%, p<0.001). Compared to non-MD-HF hospitalizations (2.01%), MD-HF hospitalizations (5.82%) were associated with significantly higher odds of inpatient mortality (OR 3.01, 95% CI: 2.03, 4.45); higher complications rate (OR 2.11, 95% CI, 1.77, 2.52) including cardiogenic shock (OR 2.61, 95% CI, 1.90, 3.59), cardiac arrest (OR 2.27, 95% CI, 1.17, 4.41), use of mechanical ventilation (OR 2.23, 95% CI, 1.82, 2.73); higher palliative care consultation (OR 4.52, 95% CI, 3.21, 6.36); as well as more extended hospital LOS (OR 1.18, 95% CI, 1.09, 1.29), higher total costs (OR 1.32, 95% CI, 1.24, 1.41), and higher odds of discharge to rehab facility (OR 2.46, 95% CI, 1.99, 3.03) and home healthcare (OR 1.85, 95% CI, 1.55, 2.21) (all p<0.001). MD was not associated with a significant difference in 30-day (OR 0.94, 95% CI, 0.78, 1.12) and 90-day (OR 0.98, 95% CI, 0.82, 1.17) all-cause readmission rates.
Conclusion: MD-HF hospitalizations were associated with higher inpatient mortality, complication rates, resource utilization, discharge to rehab facility and home healthcare, and no difference in readmission rates compared to non-MD-HF hospitalizations.
More abstracts on this topic:
A Contemporary Machine Learning-Based Risk Stratification for Mortality and Hospitalization in Heart Failure with Preserved Ejection Fraction Using Multimodal Real-World Data
Fudim Marat, Weerts Jerremy, Patel Manesh, Balu Suresh, Hintze Bradley, Torres Francisco, Micsinai Balan Mariann, Rigolli Marzia, Kessler Paul, Touzot Maxime, Lund Lars, Van Empel Vanessa, Pradhan Aruna, Butler Javed, Zehnder Tobias, Sauty Benoit, Esposito Christian, Balazard Félix, Mayer Imke, Hallal Mohammad, Loiseau Nicolas
A Case of Steroid-Refractory Immune-checkpoint-inhibitor Induced Myocarditis Responsive to Mycophenolate and Anti-thymocyte globulinDabdoub Jorge, Wilson Michael, Gottbrecht Matthew, Salazar Ryan, Shih Jeffrey