Final ID: MP572
Declining Mortality from Myocardial Infarction in Young and Middle-Aged Americans and the Impact of the COVID-19 Pandemic
Abstract Body (Do not enter title and authors here): Background: Acute myocardial infarction (AMI) represents a significant component of cardiovascular disease (CVD) mortality among the young and middle-aged populations of the United States (US).
Research Question: To analyze the long-term trends and the impact of the COVID-19 pandemic on AMI-related mortality among the young and middle-aged populations of the US.
Methods: Data from the Centers for Disease Control and Prevention Wide-ranging Online Data for Epidemiologic Research (CDC WONDER) multiple causes of death database were used to analyze death certificates from 1999 to 2023 for AMI-related deaths among the young and middle-aged population (aged 25-64) of the US. Age-adjusted mortality rates (AAMRs) per 100,000 people and associated annual percent changes (APCs) and average APC (AAPCs) were analyzed using Joinpoint regression analysis. Mortality trends were stratified by sex, race/ethnicity, and census region.
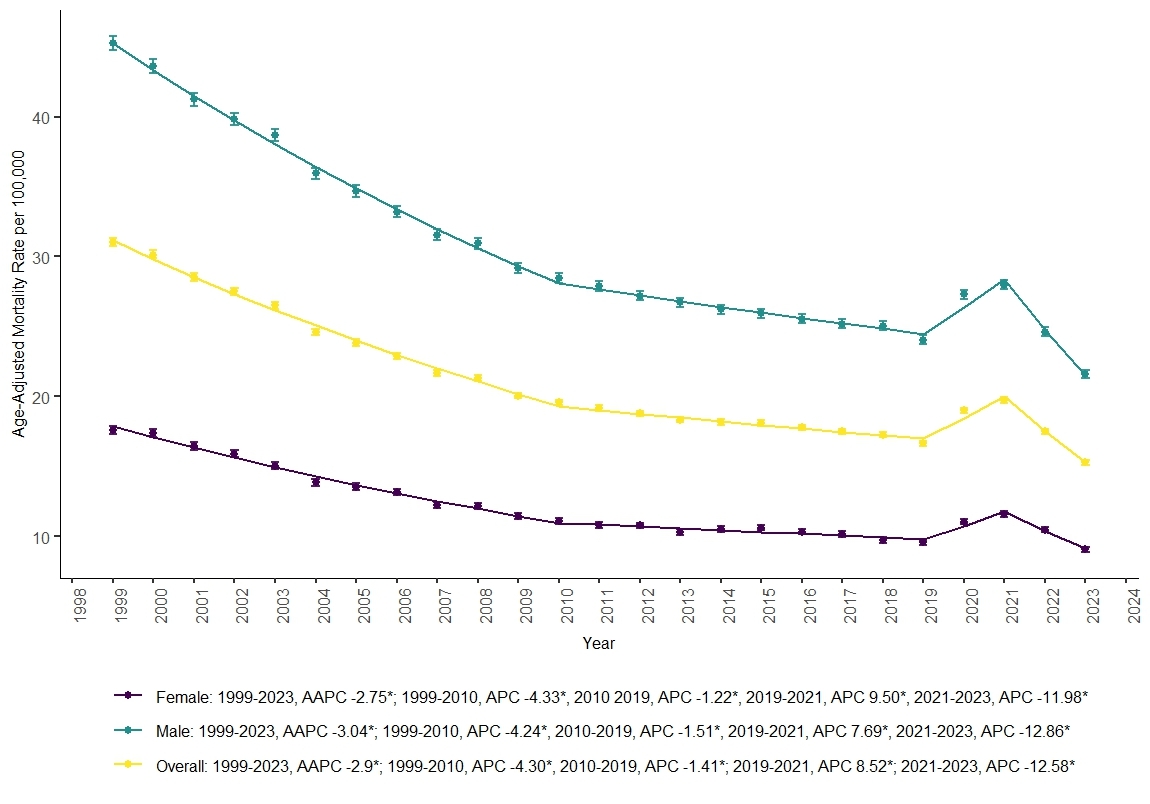
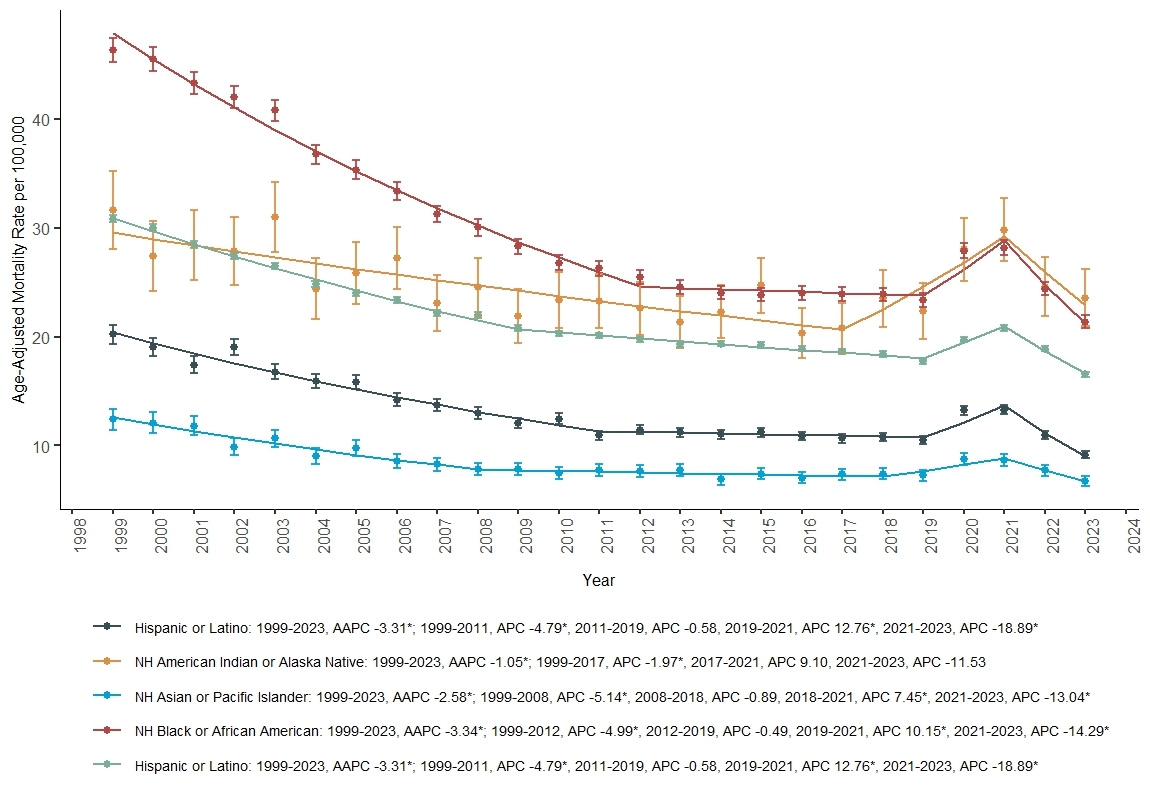
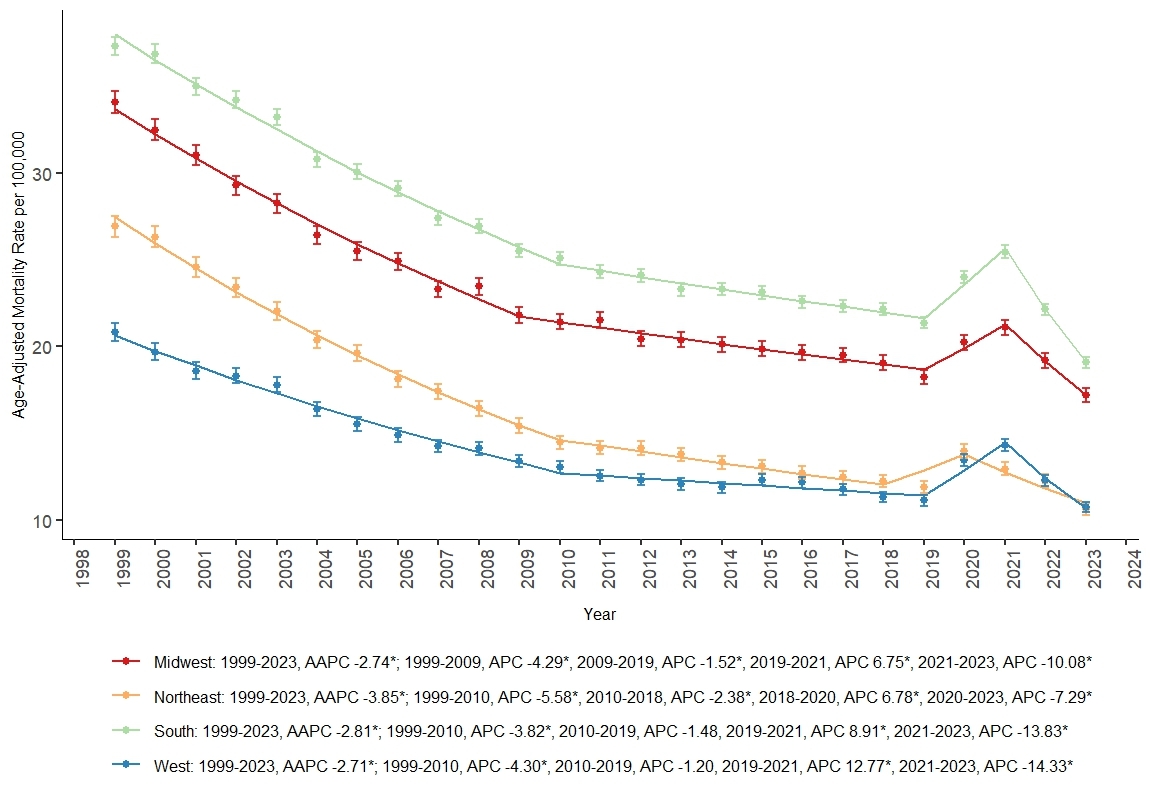
Results: From 1999 to 2023, there were 970,454 AMI-related deaths among U.S. adults aged 25-64 years. The annual number of AMI-related deaths decreased from 44,040 in 1999 to 31,522 in 2023. The overall AAMR per 100,000 decreased from 31.02 deaths (95% CI, 30.73 to 31.31) in 1999 to 15.29 (95% CI, 15.11 to 15.46) in 2023 (AAPC -2.92%, 95% CI -3.22 to -2.75). The AAMR per 100,000 declined at a faster rate from 31.02 in 1999 to 19.57 in 2010 (1999-2010, APC -4.26), followed by a slower rate from 19.57 in 2010 to 16.67 in 2019 (2010-2019, APC -1.41), The declining trend was disrupted by a transient increase during the COVID-19 pandemic, with a peak AAMR of 19.73 (95% CI, 19.53 to 19.93) in 2021 (2019-2021, APC 8.52). The declining trend resumed from 2021 to 2023, with AAMR decreasing to the lowest levels of 15.29 in 2023 (2021-2023, APC -12.58). Heterogeneity across demographic and regional groups has narrowed during these 25 years. However, they are still prevalent, with men (figure 1), non-Hispanic (NH) Black or African American, NH American Indian or Alaska Native (figure 2), and the residents of the Southern United States (figure 3) having higher mortality rates.
Conclusion: Over the past 25 years, AMI-related mortality has declined in the young and middle-aged population of the US, although rates spiked during the COVID-19 pandemic before resuming their decline in 2022. While disparities among demographic and regional groups have narrowed, they still exist, necessitating comprehensive efforts to improve cardiovascular health outcomes.
Research Question: To analyze the long-term trends and the impact of the COVID-19 pandemic on AMI-related mortality among the young and middle-aged populations of the US.
Methods: Data from the Centers for Disease Control and Prevention Wide-ranging Online Data for Epidemiologic Research (CDC WONDER) multiple causes of death database were used to analyze death certificates from 1999 to 2023 for AMI-related deaths among the young and middle-aged population (aged 25-64) of the US. Age-adjusted mortality rates (AAMRs) per 100,000 people and associated annual percent changes (APCs) and average APC (AAPCs) were analyzed using Joinpoint regression analysis. Mortality trends were stratified by sex, race/ethnicity, and census region.
Results: From 1999 to 2023, there were 970,454 AMI-related deaths among U.S. adults aged 25-64 years. The annual number of AMI-related deaths decreased from 44,040 in 1999 to 31,522 in 2023. The overall AAMR per 100,000 decreased from 31.02 deaths (95% CI, 30.73 to 31.31) in 1999 to 15.29 (95% CI, 15.11 to 15.46) in 2023 (AAPC -2.92%, 95% CI -3.22 to -2.75). The AAMR per 100,000 declined at a faster rate from 31.02 in 1999 to 19.57 in 2010 (1999-2010, APC -4.26), followed by a slower rate from 19.57 in 2010 to 16.67 in 2019 (2010-2019, APC -1.41), The declining trend was disrupted by a transient increase during the COVID-19 pandemic, with a peak AAMR of 19.73 (95% CI, 19.53 to 19.93) in 2021 (2019-2021, APC 8.52). The declining trend resumed from 2021 to 2023, with AAMR decreasing to the lowest levels of 15.29 in 2023 (2021-2023, APC -12.58). Heterogeneity across demographic and regional groups has narrowed during these 25 years. However, they are still prevalent, with men (figure 1), non-Hispanic (NH) Black or African American, NH American Indian or Alaska Native (figure 2), and the residents of the Southern United States (figure 3) having higher mortality rates.
Conclusion: Over the past 25 years, AMI-related mortality has declined in the young and middle-aged population of the US, although rates spiked during the COVID-19 pandemic before resuming their decline in 2022. While disparities among demographic and regional groups have narrowed, they still exist, necessitating comprehensive efforts to improve cardiovascular health outcomes.
More abstracts on this topic:
Achieving Guidelines within a 24-Hour Movement Paradigm and Risk of Cardiovascular Disease and All-Cause Mortality in United States Adults
Boudreaux Benjamin, Xu Chang, Dooley Erin, Hornikel Bjoern, Munson Alexandra, Shechter Ari, Palta Priya, Gabriel Kelley, Diaz Keith
Assessing Health Literacy and the Role of Race and Social Determinants in Cardiac Patients.Odigwe Celestine, Lakkis Nasser, Mayfield Hanna, Mulyala Rajasekhar, Riad Mariam, Malik Hajira, Ruiz Brent, Mulekar Madhuri, Malozzi Christopher, Omar Bassam