Final ID: MP2319
Outcomes of Heart Failure Hospitalizations in Urban Teaching vs. Non-teaching Hospitals: A Nationwide Propensity Score Matched Analysis in the United States
Abstract Body (Do not enter title and authors here): Background: Heart failure (HF) continues to be a major cause of morbidity and mortality worldwide, placing a significant burden on healthcare systems. Differences in the outcomes of HF hospitalizations for adults in teaching vs. non-teaching hospitals in urban settings are uncertain.
Research Question: Do outcomes of HF hospitalizations differ between patients hospitalized in urban teaching vs. non-teaching hospitals in the United States?
Methods: HF hospitalizations were abstracted from the 2016 through 2022 Nationwide Readmissions Database and stratified into urban teaching vs. urban non-teaching hospital settings. Propensity-score matching was used to control for baseline differences between teaching and non-teaching hospital cohorts. Logistic regression and lognormal models were estimated to assess differences in inpatient mortality, length of stay (LOS), total costs, complications, and 30-day and 90-day all-cause readmissions. Odds ratios (OR) with associated 95% Confidence intervals (CI) and p-values were reported. Analyses were conducted via SAS v. 9.4.
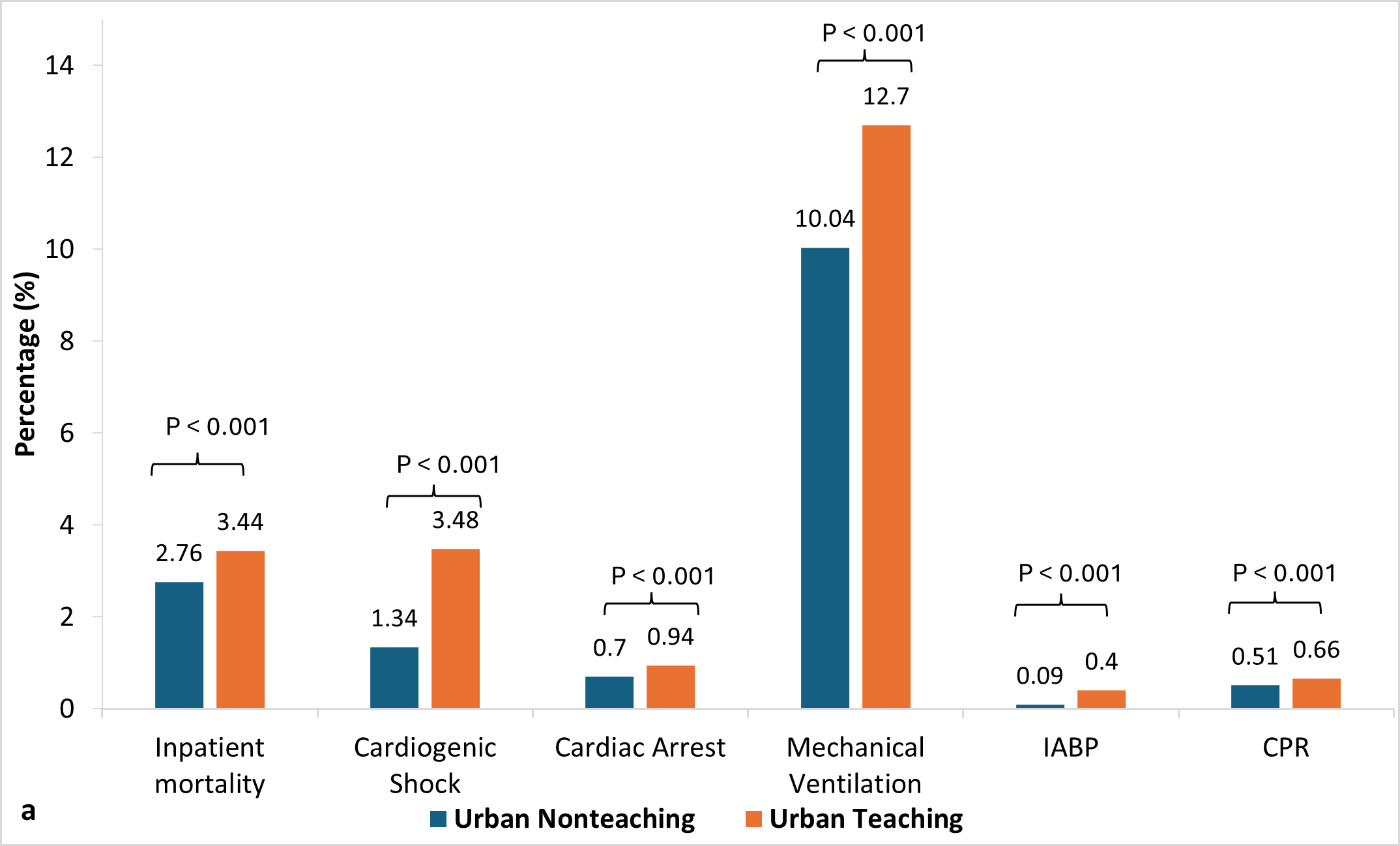
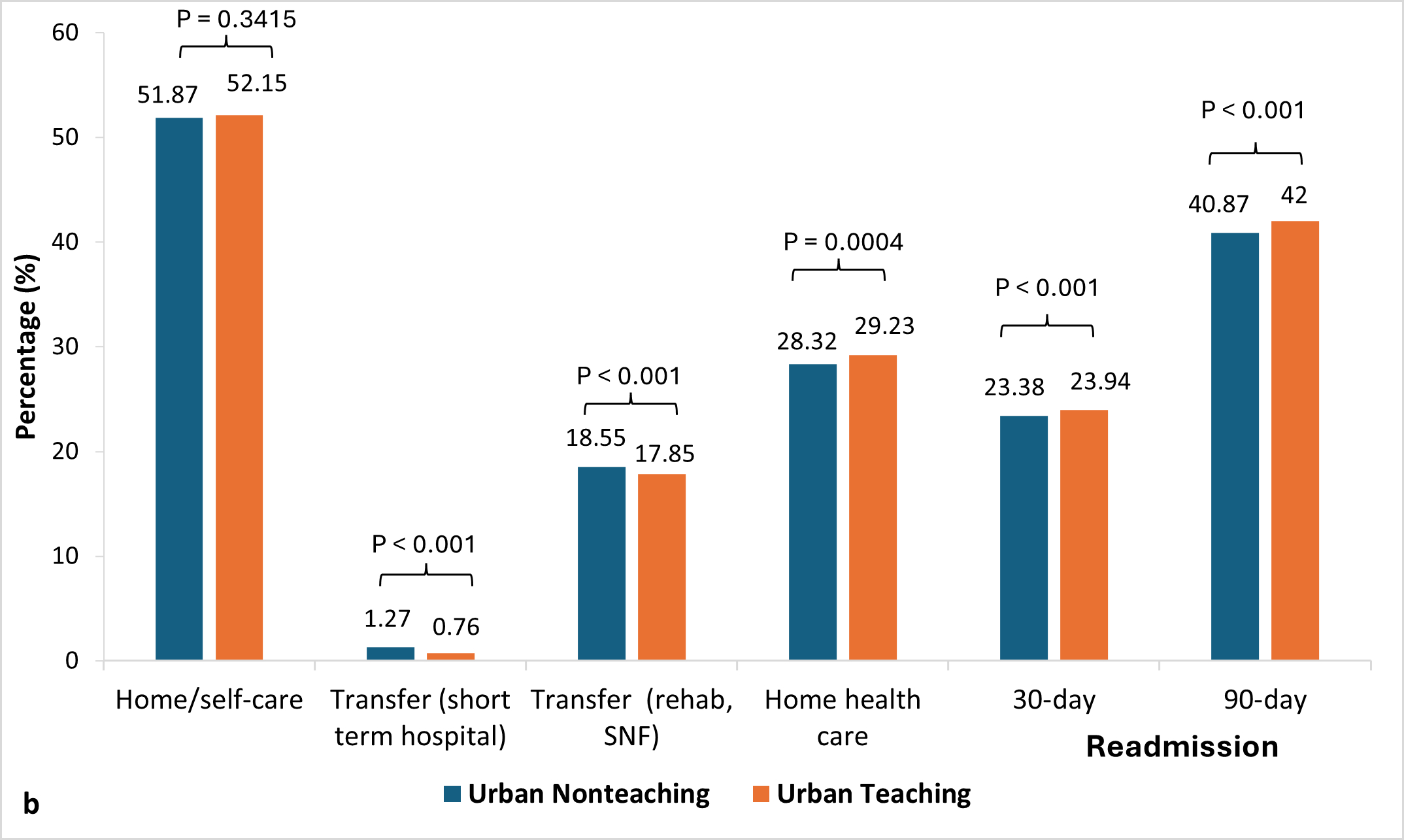
Results: A total of 7,558,299 weighted HF hospitalizations were included in the analysis, of which 76.3% involved urban teaching hospitalizations. Compared to urban non-teaching, HF hospitalizations in urban teaching hospitals were associated with higher odds of in-hospital mortality (OR 1.24, 95% CI:1.21-1.27); had higher complications, including cardiogenic shock (OR 2.58, 95% CI, 2.46, 2.70), cardiac arrest (OR 1.31, 95% CI, 1.27, 1.36), CPR (OR 1.28, 95% CI, 1.22, 1.34), and use of extracorporeal membrane oxygenation (OR 20.13, 95% CI, 13.0, 31.2), intra-aortic balloon pump (OR 4.46, 95% CI, 3.90, 5.10) and mechanical ventilation (OR 1.27, 95% CI, 1.23, 1.33); higher hospitalization cost (Ratio 1.18, 95% CI: 1.17,1.20), longer length of stay (OR 1.16, 95% CI: 1.15, 1.17) and a greater palliative care consultation rate (Ratio 1.35 (95% CI 1.30, 1.40) (all p<0.001) (Figure 1). 30-day (OR 1.03, 95% CI: 1.02, 1.04) and 90-day (OR 1.05, 95% CI: 1.02, 1.07) all-cause readmission rates were also statistically higher (p<0.001), though the difference was clinically non-significant (Figure 2). The home discharge rate was similar for teaching and non-teaching hospitals (Figure 2).
Conclusion: HF hospitalizations in urban teaching hospitals were associated with higher inpatient mortality, complication rates, resource utilization, and palliative care consult rates than urban non-teaching hospitals.
Research Question: Do outcomes of HF hospitalizations differ between patients hospitalized in urban teaching vs. non-teaching hospitals in the United States?
Methods: HF hospitalizations were abstracted from the 2016 through 2022 Nationwide Readmissions Database and stratified into urban teaching vs. urban non-teaching hospital settings. Propensity-score matching was used to control for baseline differences between teaching and non-teaching hospital cohorts. Logistic regression and lognormal models were estimated to assess differences in inpatient mortality, length of stay (LOS), total costs, complications, and 30-day and 90-day all-cause readmissions. Odds ratios (OR) with associated 95% Confidence intervals (CI) and p-values were reported. Analyses were conducted via SAS v. 9.4.
Results: A total of 7,558,299 weighted HF hospitalizations were included in the analysis, of which 76.3% involved urban teaching hospitalizations. Compared to urban non-teaching, HF hospitalizations in urban teaching hospitals were associated with higher odds of in-hospital mortality (OR 1.24, 95% CI:1.21-1.27); had higher complications, including cardiogenic shock (OR 2.58, 95% CI, 2.46, 2.70), cardiac arrest (OR 1.31, 95% CI, 1.27, 1.36), CPR (OR 1.28, 95% CI, 1.22, 1.34), and use of extracorporeal membrane oxygenation (OR 20.13, 95% CI, 13.0, 31.2), intra-aortic balloon pump (OR 4.46, 95% CI, 3.90, 5.10) and mechanical ventilation (OR 1.27, 95% CI, 1.23, 1.33); higher hospitalization cost (Ratio 1.18, 95% CI: 1.17,1.20), longer length of stay (OR 1.16, 95% CI: 1.15, 1.17) and a greater palliative care consultation rate (Ratio 1.35 (95% CI 1.30, 1.40) (all p<0.001) (Figure 1). 30-day (OR 1.03, 95% CI: 1.02, 1.04) and 90-day (OR 1.05, 95% CI: 1.02, 1.07) all-cause readmission rates were also statistically higher (p<0.001), though the difference was clinically non-significant (Figure 2). The home discharge rate was similar for teaching and non-teaching hospitals (Figure 2).
Conclusion: HF hospitalizations in urban teaching hospitals were associated with higher inpatient mortality, complication rates, resource utilization, and palliative care consult rates than urban non-teaching hospitals.
More abstracts on this topic:
A Hard Start: Early, Intensive Healthcare Utilization for Children with Critical Congenital Heart Disease
Ellis Danielle, Hall Matthew, Blume Elizabeth, Wolfe Joanne, Snaman Jennifer, Berry Jay
Prolonged In-Hospital CPR in Pediatric OHCA Patients with Estimated Poor Neurological Prognosis: Challenges in Termination Resuscitation in ChildrenNamba Takeshi, Nishikimi Mitsuaki, Kikutani Kazuya, Ohshimo Shinichiro, Shime Nobuaki