Final ID: MP1009
Outcomes of Left Atrial Appendage Occlusion Versus Direct Oral Anticoagulants in Active Cancer Patients with Atrial Fibrillation
Abstract Body (Do not enter title and authors here): Background:
Atrial fibrillation (AF) and cancer frequently co-exist, presenting a challenge due to coagulopathy, procedural needs, and elevated bleeding risk. Left atrial appendage occlusion (LAAO) may offer stroke prevention with reduced bleeding risk compared to direct oral anticoagulants (DOACs), but comparative data in cancer patients are limited.
Hypothesis:
We hypothesized that LAAO would be associated with a lower rate of major bleeding (primary endpoint) compared to DOACs in patients with AF and active cancer, without increasing the risk of thromboembolic events (TE). TE was defined as any arterial thromboembolism, TIA, or stroke. Secondary endpoints included hospitalization and all-cause mortality.
Methods:
We used the TriNetX research network to conduct a retrospective cohort study of patients ≥18 years with AF and active cancer (defined by cancer therapy within the past year). Patients treated with LAAO were compared to those on DOACs within the past 10 years. Individuals with ECOG ≥3 were excluded. Extensive propensity matching controlled for bleeding risk, comorbidities, antiplatelet use, and substance use. Outcomes were assessed at 1 and 3 years.
Results:
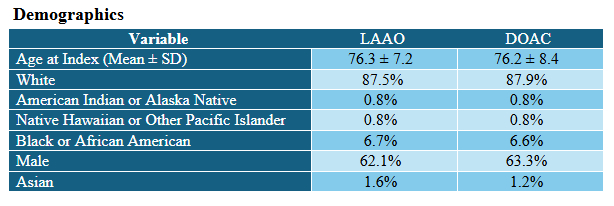
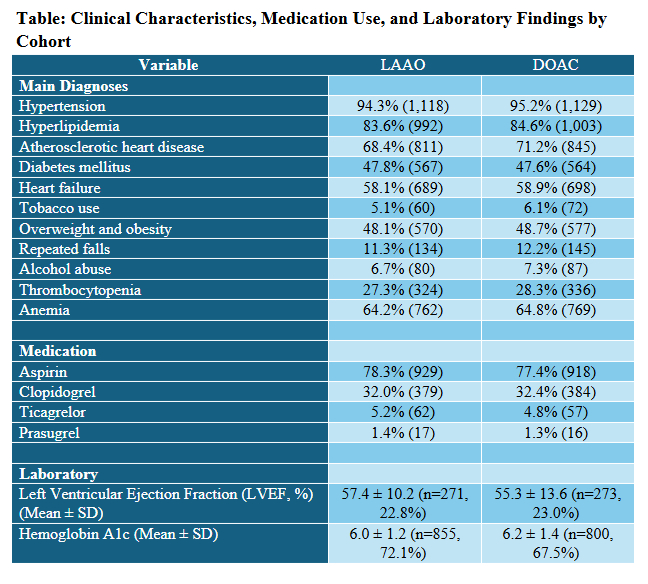
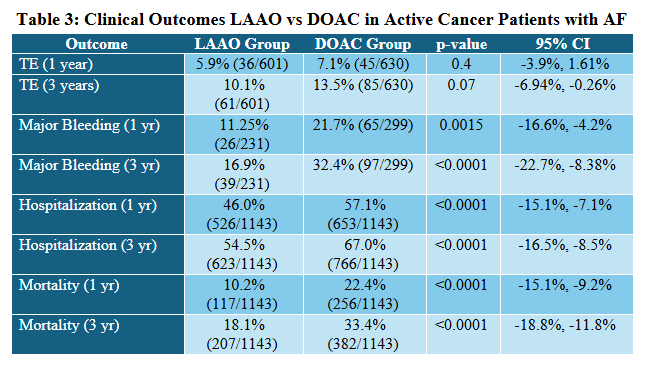
In a matched cohort study of 1,143 patients per group, rates of new TE at 1 year were 5.9% in the LAAO group versus 7.1% in the DOAC group (p=0.4), while major bleeding occurred in 11.25% vs. 21.7%, respectively (p=0.0015). At 3 years, TE rates were 10.1% vs. 13.5% (p=0.07), and major bleeding rates were 16.9% vs. 32.4% (p<0.0001). Hospitalizations and mortality were also significantly lower in the LAAO group at both time points (p<0.0001 for all). Details of demographic, clinical characteristics, and results are summarized in Tables 1, 2 , and 3, respectively.
Conclusions:
In this large real-world cohort of patients with AF and active cancer, LAAO was associated with significantly lower rates of major bleeding, hospitalization, and mortality compared to DOACs. Although the incidence of thromboembolic events was numerically lower in the LAAO group, the difference was not statistically significant. These findings suggest that LAAO may be a safer therapeutic strategy for select cancer patients at high bleeding risk, offering reduced morbidity without increasing stroke risk.
Atrial fibrillation (AF) and cancer frequently co-exist, presenting a challenge due to coagulopathy, procedural needs, and elevated bleeding risk. Left atrial appendage occlusion (LAAO) may offer stroke prevention with reduced bleeding risk compared to direct oral anticoagulants (DOACs), but comparative data in cancer patients are limited.
Hypothesis:
We hypothesized that LAAO would be associated with a lower rate of major bleeding (primary endpoint) compared to DOACs in patients with AF and active cancer, without increasing the risk of thromboembolic events (TE). TE was defined as any arterial thromboembolism, TIA, or stroke. Secondary endpoints included hospitalization and all-cause mortality.
Methods:
We used the TriNetX research network to conduct a retrospective cohort study of patients ≥18 years with AF and active cancer (defined by cancer therapy within the past year). Patients treated with LAAO were compared to those on DOACs within the past 10 years. Individuals with ECOG ≥3 were excluded. Extensive propensity matching controlled for bleeding risk, comorbidities, antiplatelet use, and substance use. Outcomes were assessed at 1 and 3 years.
Results:
In a matched cohort study of 1,143 patients per group, rates of new TE at 1 year were 5.9% in the LAAO group versus 7.1% in the DOAC group (p=0.4), while major bleeding occurred in 11.25% vs. 21.7%, respectively (p=0.0015). At 3 years, TE rates were 10.1% vs. 13.5% (p=0.07), and major bleeding rates were 16.9% vs. 32.4% (p<0.0001). Hospitalizations and mortality were also significantly lower in the LAAO group at both time points (p<0.0001 for all). Details of demographic, clinical characteristics, and results are summarized in Tables 1, 2 , and 3, respectively.
Conclusions:
In this large real-world cohort of patients with AF and active cancer, LAAO was associated with significantly lower rates of major bleeding, hospitalization, and mortality compared to DOACs. Although the incidence of thromboembolic events was numerically lower in the LAAO group, the difference was not statistically significant. These findings suggest that LAAO may be a safer therapeutic strategy for select cancer patients at high bleeding risk, offering reduced morbidity without increasing stroke risk.
More abstracts on this topic:
Adverse Events with Pulsed Field Ablation - A Review of the Food and Drug Administration’s Manufacturer and User Facility Device Experience Database
Cooper Julie, Zagrodzky William, Zagrodzky Jason, Omotoye Samuel, Sardana Mayank, Kaplan Andrew, Link Mark, Bunch Thomas, Daniels James
Association between Glucagon-like peptide-1 receptor agonists and risk of Arrhythmias: A Contemporary Real-World AnalysisJaiswal Vikash, Hanif Muhammad, Goyal Aman, Yasmin Juveria, Deb Novonil, Mashkoor Yusra, Rajak Kripa, Mattumpuram Jishanth, Weinberg Andrew