Final ID: MP2639
Impact of Anticoagulation on Outcomes of Direct Current Cardioversion in Patients with a Left Atrial Appendage Occlusion Device
Abstract Body (Do not enter title and authors here): Background:
Direct current cardioversion (DCCV) is a standard intervention for restoring sinus rhythm in atrial fibrillation (AF). Left atrial appendage closure (LAAC) devices provide an alternative to anticoagulation (AC) for stroke prevention in select AF patients, but their effectiveness in mitigating thromboembolic complications during and after DCCV remains uncertain. This study evaluates the outcomes of DCCV in patients with LAAC devices in those receiving AC and those who are not.
Methods:
This was a retrospective observational cohort study using de-identified electronic health records from the TriNetX Research Network, including 103 healthcare organizations across the United States. The study included patients who underwent DCCV at least 6 months after LAAC device implantation. Patients with prior stroke, transient ischemic attack (TIA), hypertrophic cardiomyopathy, deep vein thrombosis, or pulmonary embolism were excluded.
The primary exposure was AC use from 1 day prior to 1 month post-DCCV. The primary thromboembolic outcome was a composite of stroke, TIA, and arterial thromboembolism. The primary bleeding outcome was a composite of gastrointestinal, intracranial, genitourinary, and other bleeding events. Follow-up time was 1 year. Propensity score matching (1:1) was used to control for confounders including age, sex, hypertension, heart failure, ischemic heart disease, and diabetes. Risk ratios (RRs) and 95% confidence intervals (CIs) were calculated.
Results:
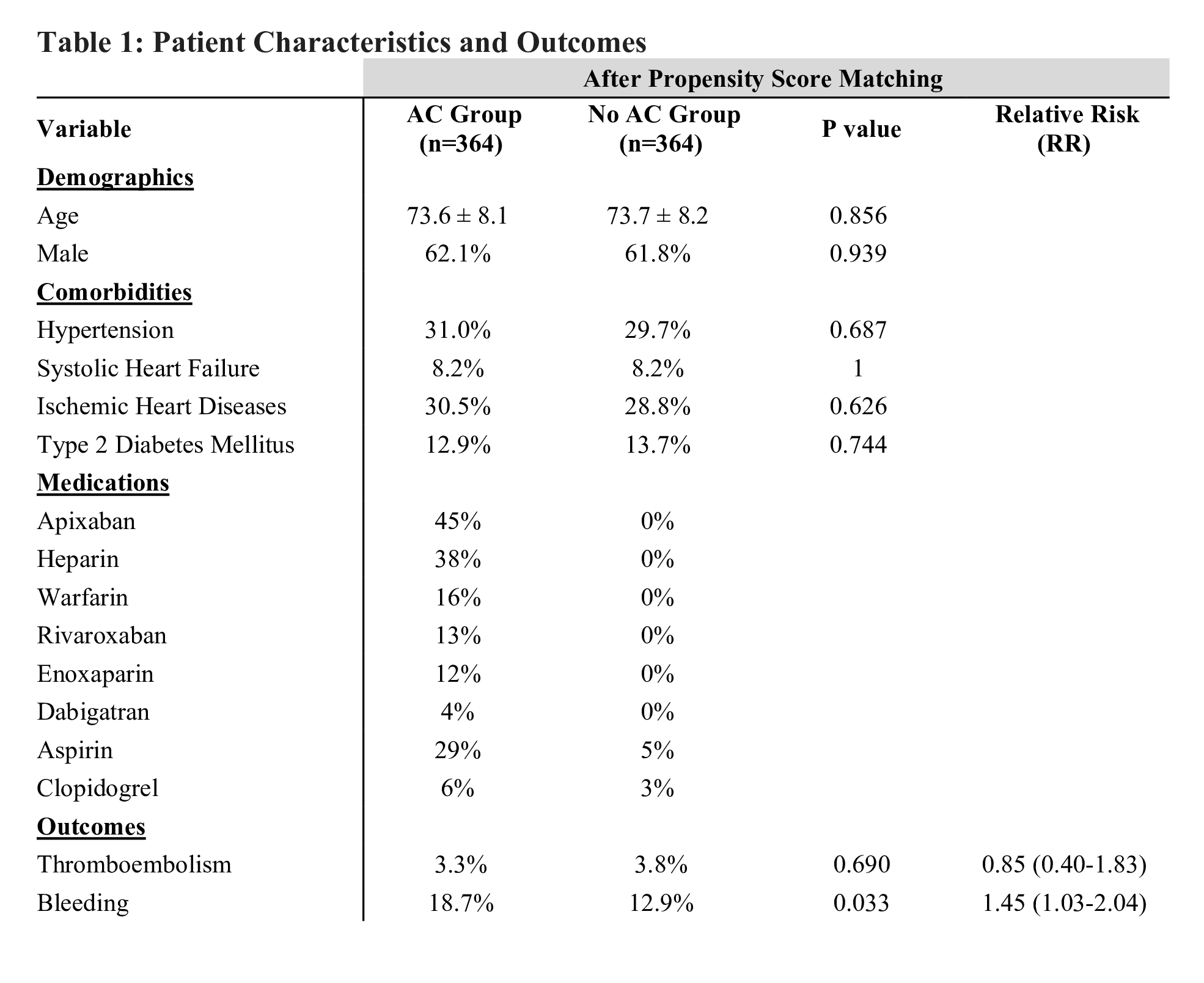
Of 1,295 patients identified, 925 received AC and 370 did not. After propensity score matching, 364 patients remained in each group. The mean age was 73.6 ± 8.1 years and 62% were male.
At 1 year, the composite thromboembolic event rate was 3.3% in the AC group and 3.8% in the non-AC group (RR 0.86; 95% CI 0.40–1.83; p=0.690). Bleeding events occurred more frequently in the AC group (18.7%) than in the non-AC group (12.9%) (RR 1.45; 95% CI 1.03–2.04; p=0.033).
Conclusions:
In patients with LAAC devices undergoing DCCV, the omission of routine periprocedural AC did not increase thromboembolic risk but was associated with fewer bleeding complications. Selective use of AC may be appropriate, especially when a stable device seal is confirmed. Further prospective studies are warranted to define standardized management protocols.
Direct current cardioversion (DCCV) is a standard intervention for restoring sinus rhythm in atrial fibrillation (AF). Left atrial appendage closure (LAAC) devices provide an alternative to anticoagulation (AC) for stroke prevention in select AF patients, but their effectiveness in mitigating thromboembolic complications during and after DCCV remains uncertain. This study evaluates the outcomes of DCCV in patients with LAAC devices in those receiving AC and those who are not.
Methods:
This was a retrospective observational cohort study using de-identified electronic health records from the TriNetX Research Network, including 103 healthcare organizations across the United States. The study included patients who underwent DCCV at least 6 months after LAAC device implantation. Patients with prior stroke, transient ischemic attack (TIA), hypertrophic cardiomyopathy, deep vein thrombosis, or pulmonary embolism were excluded.
The primary exposure was AC use from 1 day prior to 1 month post-DCCV. The primary thromboembolic outcome was a composite of stroke, TIA, and arterial thromboembolism. The primary bleeding outcome was a composite of gastrointestinal, intracranial, genitourinary, and other bleeding events. Follow-up time was 1 year. Propensity score matching (1:1) was used to control for confounders including age, sex, hypertension, heart failure, ischemic heart disease, and diabetes. Risk ratios (RRs) and 95% confidence intervals (CIs) were calculated.
Results:
Of 1,295 patients identified, 925 received AC and 370 did not. After propensity score matching, 364 patients remained in each group. The mean age was 73.6 ± 8.1 years and 62% were male.
At 1 year, the composite thromboembolic event rate was 3.3% in the AC group and 3.8% in the non-AC group (RR 0.86; 95% CI 0.40–1.83; p=0.690). Bleeding events occurred more frequently in the AC group (18.7%) than in the non-AC group (12.9%) (RR 1.45; 95% CI 1.03–2.04; p=0.033).
Conclusions:
In patients with LAAC devices undergoing DCCV, the omission of routine periprocedural AC did not increase thromboembolic risk but was associated with fewer bleeding complications. Selective use of AC may be appropriate, especially when a stable device seal is confirmed. Further prospective studies are warranted to define standardized management protocols.
More abstracts on this topic:
A Contactless and Automated Approach to the Acute Stroke Assessment
Saadat Moh, Titus Ryan, Verkuilen Haley, Fleming Phil, Sur Sanjib, Sen Souvik
A ChatGLM-based stroke diagnosis and prediction toolSong Xiaowei, Wang Jiayi, Ma Weizhi, Wu Jian, Wang Yueming, Gao Ceshu, Wei Chenming, Pi Jingtao