Final ID: Su4100
Association of Antiphospholipid Syndrome with Infective Endocarditis and Staphylococcal Sepsis: A U.S. Nationwide Inpatient Sample Analysis
Abstract Body (Do not enter title and authors here): Background: Antiphospholipid syndrome (APS) predisposes patients to thrombosis and cardiac valve lesions (e.g., Libman-Sacks endocarditis). These vegetations, though sterile, may serve as a nidus for infection. The risk of infective endocarditis (IE) and other serious infections in APS patients within large populations remains poorly quantified, representing a key knowledge gap.
Research Questions/Hypothesis: To quantify the risk of the primary outcome, IE, and secondary outcomes of MRSA sepsis and MSSA sepsis, associated with APS using a large, nationally representative inpatient database.
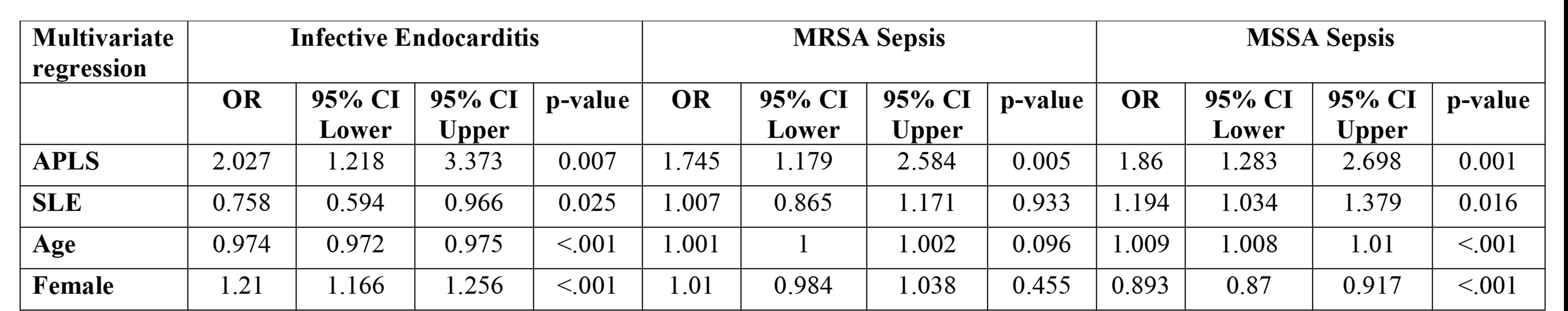
Methods/Approach: This retrospective cross-sectional study utilized the Nationwide Inpatient Sample (NIS) database from 2016 to 2020. Hospitalized patients aged 18-75 with APS were compared to those without APS. Patients with major pre-existing risks for IE or significant confounders (e.g., prosthetic valves, specific congenital/rheumatic heart diseases, ESRD) were excluded. Multivariable logistic regression was used to calculate adjusted odds ratios (aORs) with 95% confidence intervals (CIs), adjusting for age, sex, race/ethnicity, hospital region, primary payer, median household income, and Systemic Lupus Erythematosus (SLE) status.
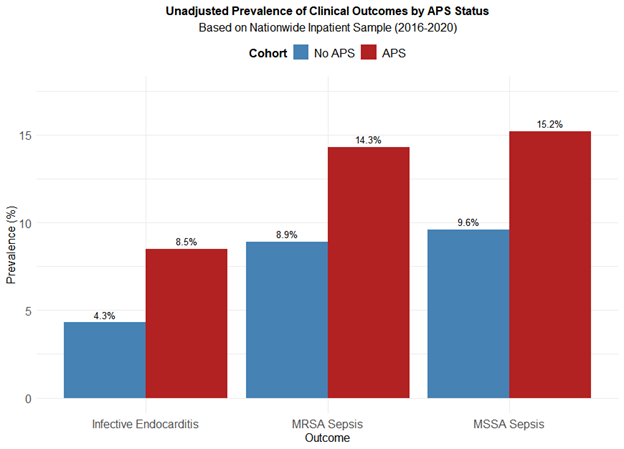
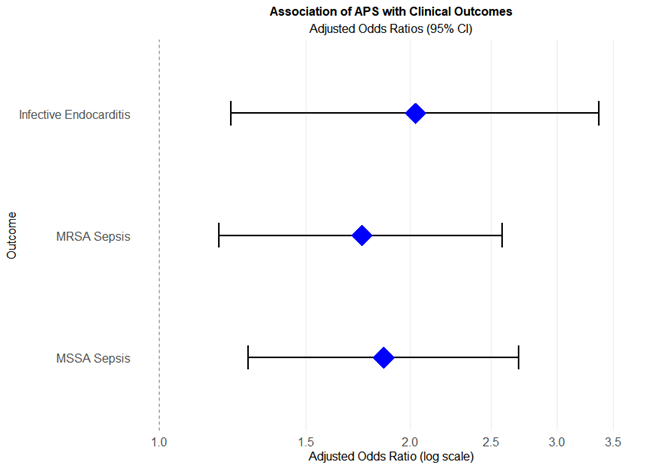
Results/Data: A total of 297,459 patients met inclusion criteria; 223 hospitalizations (0.075%) had an APS diagnosis. APS patients were significantly younger (mean age 46.9 ± 14.4 vs. 50.8 ± 14.6 years, p<0.001) and more often female (72.6% vs. 40.0%, p<0.001). Unadjusted analyses revealed higher IE prevalence in APS (8.5% vs. 4.3%, p = 0.002), MRSA sepsis (14.3% vs. 8.9%, p = 0.004), and MSSA sepsis (15.2% vs. 9.6%, p = 0.004). In multivariable analysis, APS was significantly associated with over double the odds of IE (aOR 2.03; 95% CI 1.22–3.37; p = 0.007). APS also conferred increased risks of MRSA sepsis (aOR 1.75; 95% CI 1.18–2.58; p=0.005) and MSSA sepsis (aOR 1.86; 95% CI 1.28–2.70; p=0.001). In-hospital mortality within the IE cohort was not significantly different (0.2% vs. 0.1%, p = 0.543).
Conclusion(s): APS emerged as a significant independent risk factor for IE, MRSA, and MSSA sepsis in this nationwide analysis. These findings suggest a broader vulnerability to infection in APS, highlighting the critical need for increased clinical suspicion, vigilant monitoring, and potentially tailored prophylactic or treatment approaches for severe infections in these patients.
Research Questions/Hypothesis: To quantify the risk of the primary outcome, IE, and secondary outcomes of MRSA sepsis and MSSA sepsis, associated with APS using a large, nationally representative inpatient database.
Methods/Approach: This retrospective cross-sectional study utilized the Nationwide Inpatient Sample (NIS) database from 2016 to 2020. Hospitalized patients aged 18-75 with APS were compared to those without APS. Patients with major pre-existing risks for IE or significant confounders (e.g., prosthetic valves, specific congenital/rheumatic heart diseases, ESRD) were excluded. Multivariable logistic regression was used to calculate adjusted odds ratios (aORs) with 95% confidence intervals (CIs), adjusting for age, sex, race/ethnicity, hospital region, primary payer, median household income, and Systemic Lupus Erythematosus (SLE) status.
Results/Data: A total of 297,459 patients met inclusion criteria; 223 hospitalizations (0.075%) had an APS diagnosis. APS patients were significantly younger (mean age 46.9 ± 14.4 vs. 50.8 ± 14.6 years, p<0.001) and more often female (72.6% vs. 40.0%, p<0.001). Unadjusted analyses revealed higher IE prevalence in APS (8.5% vs. 4.3%, p = 0.002), MRSA sepsis (14.3% vs. 8.9%, p = 0.004), and MSSA sepsis (15.2% vs. 9.6%, p = 0.004). In multivariable analysis, APS was significantly associated with over double the odds of IE (aOR 2.03; 95% CI 1.22–3.37; p = 0.007). APS also conferred increased risks of MRSA sepsis (aOR 1.75; 95% CI 1.18–2.58; p=0.005) and MSSA sepsis (aOR 1.86; 95% CI 1.28–2.70; p=0.001). In-hospital mortality within the IE cohort was not significantly different (0.2% vs. 0.1%, p = 0.543).
Conclusion(s): APS emerged as a significant independent risk factor for IE, MRSA, and MSSA sepsis in this nationwide analysis. These findings suggest a broader vulnerability to infection in APS, highlighting the critical need for increased clinical suspicion, vigilant monitoring, and potentially tailored prophylactic or treatment approaches for severe infections in these patients.
More abstracts on this topic:
Adoptive Transfer of Lupus Patient PBMCs Promotes Salt-Sensitive Hypertension and Kidney Injury in Immunodeficient Mice
Saleem Mohammad, Ormseth Michelle, Kirabo Annet, Ahmad Taseer, Haynes Alexandria, Albritton Claude, Arshad Suha, Kulapatana Phicharmon, Posey Olivia, Major Amy, Stein Charles
A New Comprehensive Parameter Residual C-Reactive Protein And Neutrophil Risk Predict Adverse Events In Chinese Patients After Percutaneous Coronary Intervention: a National Multi-Center Prospective Cohort StudyYang Fen, Yu Miao, Cheng Xiang