Final ID: MP1173
Relationship between heart function, fibrosis and AT1 receptors in the heart and the kidneys of a mouse model of doxorubicin-induced cardiomyopathy
Abstract Body (Do not enter title and authors here): Introduction: Ivabradine (IVAB) is an effective heart-rate lowering drug used in patients with heart failure. However, its potential protective effect in the context of doxorubicin (DOXO)-induced cardiomyopathy, a serious complication of anthracycline chemotherapy, remain poorly understood.
Aims: 1) To assess the effects of IVAB on cardiac remodeling in a murine model of DOXO-induced cardiomyopathy, and 2) to investigate its potential interaction with the renin-angiotensin system, as the cardioprotective effects of IVAB may extend beyond heart rate reduction.
Methods: C57BLC/6 female mice (n=36) were allocated into 2 groups: control (n=4) and treatment by DOXO (n=32). DOXO administration (4 mg/kg/week, intraperitoneal injections) was performed over 5 weeks and followed by a 10 weeks gavage treatment with either water (H2O), IVAB (10 mg/kg/day), or metoprolol (METO) (100 mg/kg/day). Heart function was assessed by echocardiography every two weeks over a 16-week period. At the end of the study, fibrosis levels and angiotensin II type 1 receptor (AT1R) expression in the heart and kidneys were evaluated using picrosirius red (PSR) staining and in vitro 125I-[Sar1, Ile8]-Angiotensin II autoradiography, respectively. Statistical analyses were conducted using One-Way ANOVA and paired t-tests.
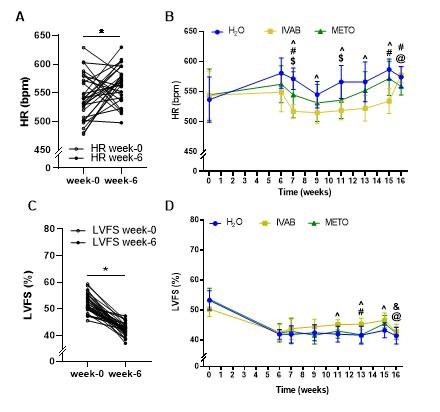
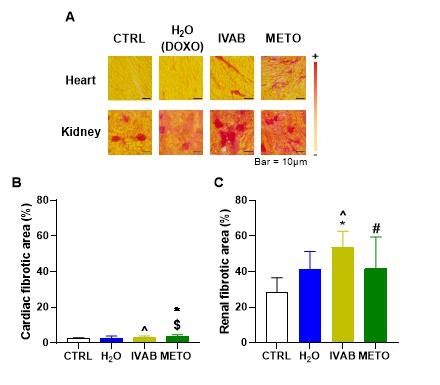
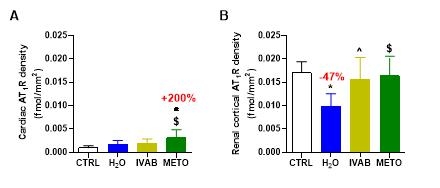
Results: After completion of DOXO injections, all mice demonstrated a lower cardiac function versus baseline (-19%, p<0.0001) and higher heart rate (+5%, p<0.05). During treatment, only IVAB reduced heart rate (-9%, p<0.0001) and improved the cardiac function (+8%, p<0.05) when compared to H2O group. One week after treatment completion, 1) cardiac function in IVAB group was decreased (-8%, p<0.01) when compared to end of treatment; and was similar to the other groups; 2) there was no difference in cardiac mass between groups; 3) cardiac fibrosis was increased in METO (+40%, p<0.05) when compared to control; 4) renal fibrosis was increased in all DOXO-groups vs controls (H2O +47%, p=0.055; IVAB +90%, p<0.001 and METO +47%, p=0.058); and 5) renal AT1Rs were reduced (-47%, p<0.01) only in the DOXO-H2O group, while treatment with IVAB and METO preserved these levels at values comparable to controls.
Conclusions: Improved cardiac function by IVAB is not due to reduced fibrosis, despite sustained normal renal AT1R expression. This may explain the rapid relapse in cardiac dysfunction once the drug is stopped.
Aims: 1) To assess the effects of IVAB on cardiac remodeling in a murine model of DOXO-induced cardiomyopathy, and 2) to investigate its potential interaction with the renin-angiotensin system, as the cardioprotective effects of IVAB may extend beyond heart rate reduction.
Methods: C57BLC/6 female mice (n=36) were allocated into 2 groups: control (n=4) and treatment by DOXO (n=32). DOXO administration (4 mg/kg/week, intraperitoneal injections) was performed over 5 weeks and followed by a 10 weeks gavage treatment with either water (H2O), IVAB (10 mg/kg/day), or metoprolol (METO) (100 mg/kg/day). Heart function was assessed by echocardiography every two weeks over a 16-week period. At the end of the study, fibrosis levels and angiotensin II type 1 receptor (AT1R) expression in the heart and kidneys were evaluated using picrosirius red (PSR) staining and in vitro 125I-[Sar1, Ile8]-Angiotensin II autoradiography, respectively. Statistical analyses were conducted using One-Way ANOVA and paired t-tests.
Results: After completion of DOXO injections, all mice demonstrated a lower cardiac function versus baseline (-19%, p<0.0001) and higher heart rate (+5%, p<0.05). During treatment, only IVAB reduced heart rate (-9%, p<0.0001) and improved the cardiac function (+8%, p<0.05) when compared to H2O group. One week after treatment completion, 1) cardiac function in IVAB group was decreased (-8%, p<0.01) when compared to end of treatment; and was similar to the other groups; 2) there was no difference in cardiac mass between groups; 3) cardiac fibrosis was increased in METO (+40%, p<0.05) when compared to control; 4) renal fibrosis was increased in all DOXO-groups vs controls (H2O +47%, p=0.055; IVAB +90%, p<0.001 and METO +47%, p=0.058); and 5) renal AT1Rs were reduced (-47%, p<0.01) only in the DOXO-H2O group, while treatment with IVAB and METO preserved these levels at values comparable to controls.
Conclusions: Improved cardiac function by IVAB is not due to reduced fibrosis, despite sustained normal renal AT1R expression. This may explain the rapid relapse in cardiac dysfunction once the drug is stopped.
More abstracts on this topic:
A Competency-Based Screening Echocardiography Curriculum Designed for Rural American Indian Community Health Representatives
Thoroughman Rose, Riley Alan, De Loizaga Sarah, Adams David, Beaton Andrea, Buonfiglio Samantha, Danforth Kristen, Masyuko Sarah, Miller Mccall, Yadava Mrinal
A-band titin-truncating variant promotes the development of arrhythmia-induced cardiomyopathy in a novel genetically-engineered porcine modelLee Kwonjae, Del Rio Carlos, Mcnally Elizabeth, Pfenniger Anna, Bhatnagar Ashita, Glinton Kristofor, Burrell Amy, Ober Rebecca, Mcluckie Alicia, Bishop Brian, Rogers Christopher, Geist Gail