Final ID: MP1901
Recurrent PEA Arrests due to Coronary Vasospasm in the Absence of Obstructive CAD
Abstract Body (Do not enter title and authors here): Introduction:
Coronary vasospasm is a transient, reversible narrowing of the coronary arteries that may lead to myocardial ischemia, arrhythmias, or cardiac arrest. Diagnosis is particularly challenging in patients without obstructive coronary artery disease and in the context of critical illness.
Case Presentation:
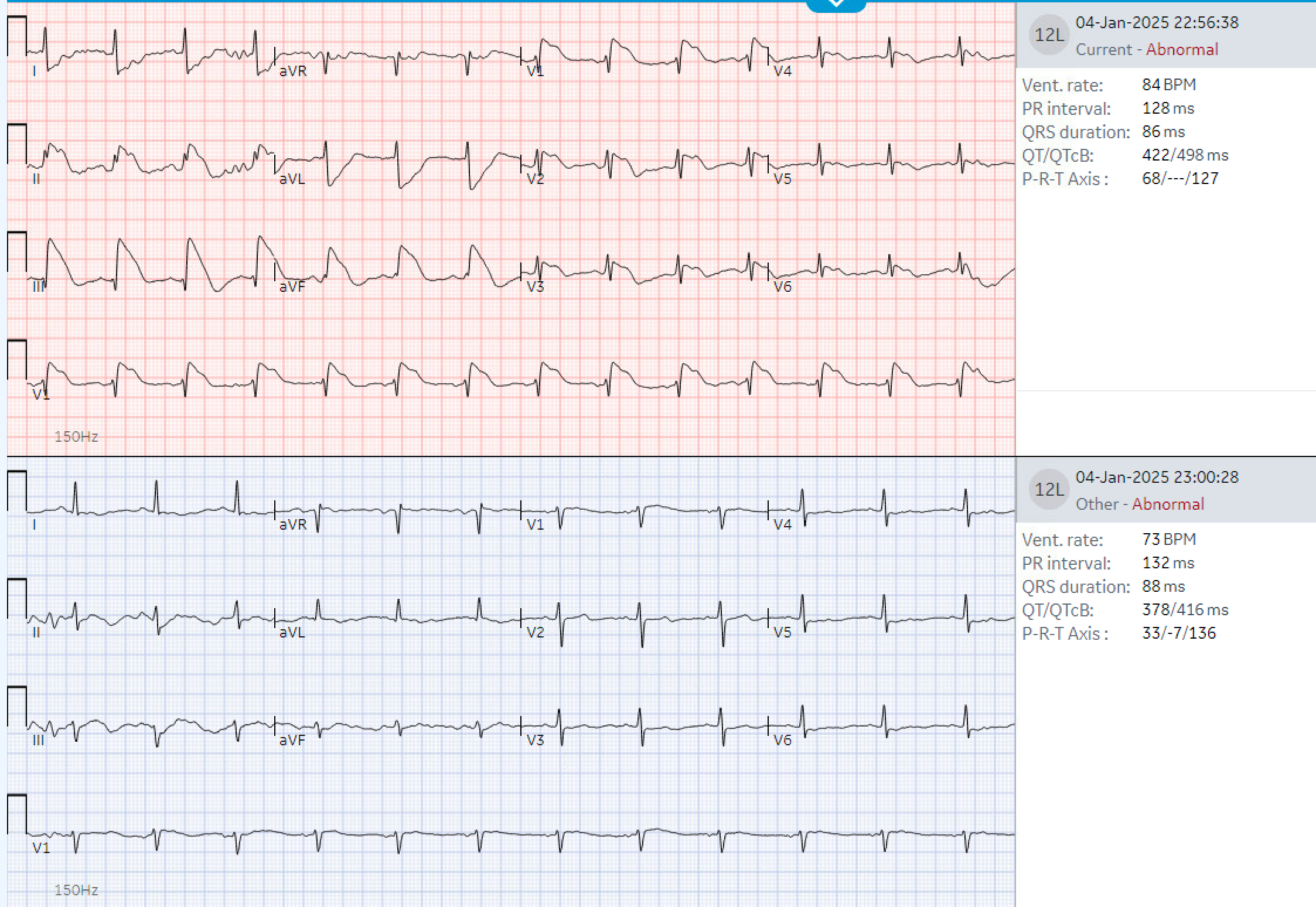
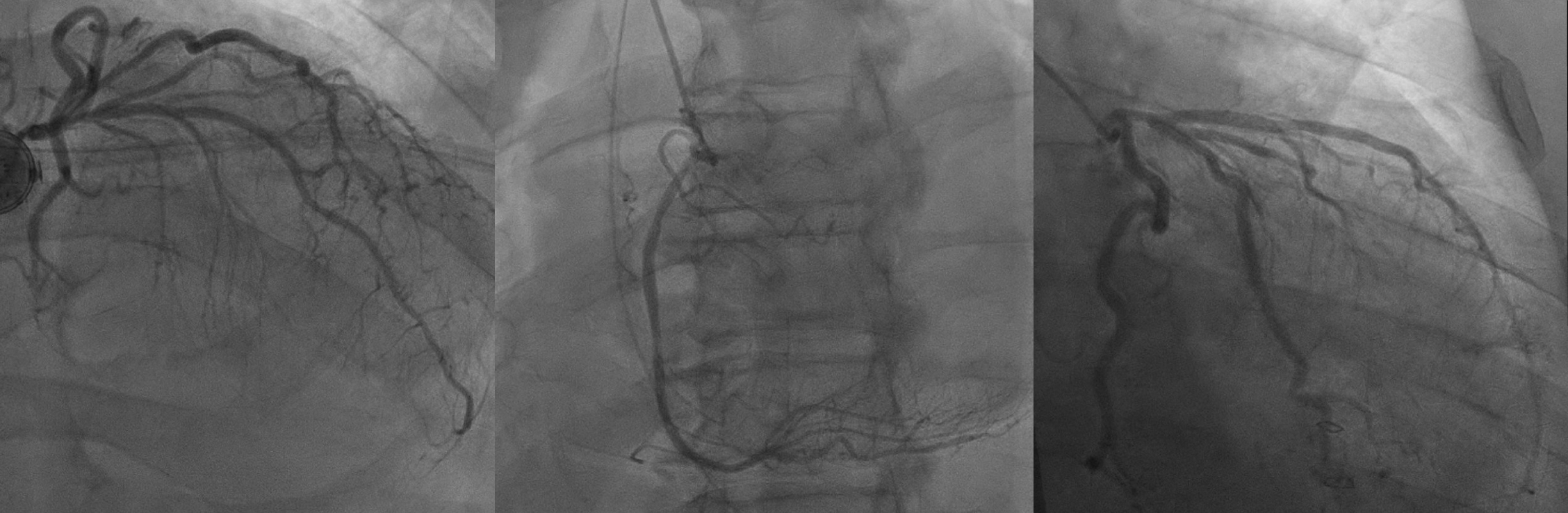
We present the case of a 68-year-old male with cirrhosis and hepatocellular carcinoma who developed multiple episodes of pulseless electrical activity (PEA) arrest following emergent abdominal surgery. The patient underwent electrocardiography, echocardiography, and coronary angiography. Clinical findings were reviewed alongside laboratory and imaging data to identify a unifying cause.
Post-arrest echocardiography demonstrated a reduced ejection fraction with anterior and apical akinesis. Coronary angiography showed no critical lesions but revealed subtle luminal irregularities in the LAD. The patient experienced multiple episodes of QRS widening, ST changes, hypotension, and PEA arrest—all transient and resolving within minutes. Electrolytes were largely normal. Coronary vasospasm was suspected based on episodic ischemic ECG changes, angiographic findings, and lack of metabolic or structural explanations. The patient was managed with intravenous nitroglycerin, later transitioned to clevidipine, with vasopressor support using norepinephrine. After initiating anti-vasospastic therapy, ischemic episodes and arrests abated. Repeat TTE redemonstrated LV concentric remodeling, hyperdynamic systolic function with recovered EF.
Discussion:
This case highlights coronary vasospasm as a reversible but potentially fatal cause of cardiac arrest in the absence of obstructive disease. In critically ill patients, coronary vasospasm may be triggered by a combination of surgical stress, systemic inflammation, sympathetic overactivity, and the use of vasoconstrictive agents such as vasopressors or certain anesthetics. Patients with liver disease are especially susceptible due to impaired autonomic regulation and endothelial dysfunction. These factors collectively heighten vascular reactivity, creating a permissive environment for vasospasm even without obstructive coronary disease. Particularly in post-op, critically patients with transient ischemic episodes, vasospasm should be considered early. Prompt diagnosis and vasodilator therapy are key to improving outcomes in this high-risk population.
Coronary vasospasm is a transient, reversible narrowing of the coronary arteries that may lead to myocardial ischemia, arrhythmias, or cardiac arrest. Diagnosis is particularly challenging in patients without obstructive coronary artery disease and in the context of critical illness.
Case Presentation:
We present the case of a 68-year-old male with cirrhosis and hepatocellular carcinoma who developed multiple episodes of pulseless electrical activity (PEA) arrest following emergent abdominal surgery. The patient underwent electrocardiography, echocardiography, and coronary angiography. Clinical findings were reviewed alongside laboratory and imaging data to identify a unifying cause.
Post-arrest echocardiography demonstrated a reduced ejection fraction with anterior and apical akinesis. Coronary angiography showed no critical lesions but revealed subtle luminal irregularities in the LAD. The patient experienced multiple episodes of QRS widening, ST changes, hypotension, and PEA arrest—all transient and resolving within minutes. Electrolytes were largely normal. Coronary vasospasm was suspected based on episodic ischemic ECG changes, angiographic findings, and lack of metabolic or structural explanations. The patient was managed with intravenous nitroglycerin, later transitioned to clevidipine, with vasopressor support using norepinephrine. After initiating anti-vasospastic therapy, ischemic episodes and arrests abated. Repeat TTE redemonstrated LV concentric remodeling, hyperdynamic systolic function with recovered EF.
Discussion:
This case highlights coronary vasospasm as a reversible but potentially fatal cause of cardiac arrest in the absence of obstructive disease. In critically ill patients, coronary vasospasm may be triggered by a combination of surgical stress, systemic inflammation, sympathetic overactivity, and the use of vasoconstrictive agents such as vasopressors or certain anesthetics. Patients with liver disease are especially susceptible due to impaired autonomic regulation and endothelial dysfunction. These factors collectively heighten vascular reactivity, creating a permissive environment for vasospasm even without obstructive coronary disease. Particularly in post-op, critically patients with transient ischemic episodes, vasospasm should be considered early. Prompt diagnosis and vasodilator therapy are key to improving outcomes in this high-risk population.
More abstracts on this topic:
An Observation Of Racial Disparities In Patients Admitted With St Segment Elevated Myocardial Elevation
Ajenaghughrure Godbless, Rahima Kenan, Shemisa Kamal, Mishra Aavash, Kishore Gehna
A Case of Successful Resuscitation After Out-of-hospital Cardiac Arrest Caused by Undiagnosed Pheochromocytoma-induced CardiomyopathyHatakeyama Toshihiro, Suetsugu Yusuke, Watanabe Kaoru, Matsushima Hisao