Final ID: MP1940
An Unlikely Host: A Rare Case of Streptococcus Pneumoniae Purulent Pericarditis in an Immunocompetent Patient
Abstract Body (Do not enter title and authors here): Introduction:
Purulent pericarditis is a rare, potentially fatal infection characterized by pus in the pericardial space. The most common culprit is streptococcus pneumoniae, and it typically occurs in immunocompromised patients. This case highlights pneumococcal purulent pericarditis in an immunocompetent patient who presented with pneumonia and recent chest trauma.
Case Description:
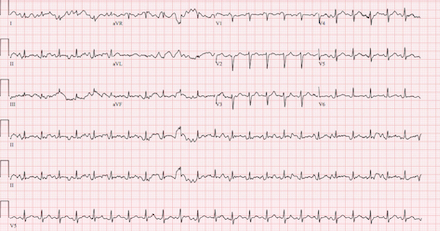
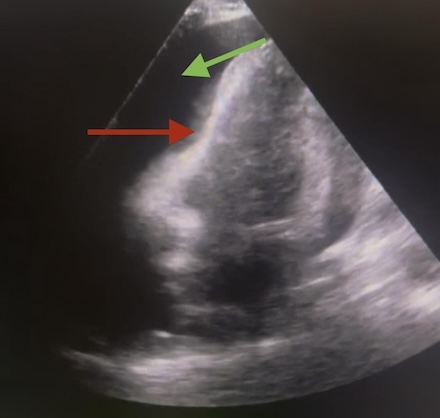
A 45-year-old male with hypertension presented with chest pain, cough, and malaise. Chest computerized tomography (CT) revealed right upper lobe pneumonia and several acute and chronic rib fractures. He was tachycardic, febrile (102.9°F), and hypoxic. Labs showed leukocytosis (19.8) and elevated lactate (2.5). Electrocardiogram demonstrated low voltage (Figure A). Bedside trans thoracic echocardiogram (TTE) showed large pericardial effusion with right ventricular collapse (Figure B). Thus, a drain was placed, releasing 850 mL of purulent fluid. Post drainage, formal TTE revealed small residual effusion (Figure C). Vancomycin, cefepime, and metronidazole were started. Fluid studies showed 32,000 cells (91% neutrophils). Fluid cultures grew streptococcus pneumoniae. By day seven, the drain produced less than 50 mL over the previous twenty four hours. Bedside echocardiogram was confirmatory, so the drain was removed. The patient was discharged on six weeks of cefuroxime and a three month course of colchicine.
Discussion:
Although our patient endorsed chest pain, he did not demonstrate classic pericarditis signs. Unlike non infectious acute pericarditis, purulent pericarditis typically manifests as fever, tachycardia, and workup that parallels sepsis, highlighting the importance of comprehensive workup. In his case, purulent pericarditis likely resulted from contiguous spread of bacterial pneumonia, the most common route by which streptococcus pneumoniae enters the pericardium. While purulent pericarditis typically affects immunocompromised patients, our immunocompetent patient had recent chest trauma, which likely increased susceptibility by creating a pro inflammatory state. Prompt drainage and antibiotics were essential, as untreated purulent pericarditis mortality is near 100%. Even with correct treatment, mortality can reach up to 30%.
Conclusion:
Even in immunocompetent states, providers should consider purulent pericarditis especially when patients present with sepsis and concerns for pericardial effusion. Early recognition, drainage, and antibiotics are critical to survival.
Purulent pericarditis is a rare, potentially fatal infection characterized by pus in the pericardial space. The most common culprit is streptococcus pneumoniae, and it typically occurs in immunocompromised patients. This case highlights pneumococcal purulent pericarditis in an immunocompetent patient who presented with pneumonia and recent chest trauma.
Case Description:
A 45-year-old male with hypertension presented with chest pain, cough, and malaise. Chest computerized tomography (CT) revealed right upper lobe pneumonia and several acute and chronic rib fractures. He was tachycardic, febrile (102.9°F), and hypoxic. Labs showed leukocytosis (19.8) and elevated lactate (2.5). Electrocardiogram demonstrated low voltage (Figure A). Bedside trans thoracic echocardiogram (TTE) showed large pericardial effusion with right ventricular collapse (Figure B). Thus, a drain was placed, releasing 850 mL of purulent fluid. Post drainage, formal TTE revealed small residual effusion (Figure C). Vancomycin, cefepime, and metronidazole were started. Fluid studies showed 32,000 cells (91% neutrophils). Fluid cultures grew streptococcus pneumoniae. By day seven, the drain produced less than 50 mL over the previous twenty four hours. Bedside echocardiogram was confirmatory, so the drain was removed. The patient was discharged on six weeks of cefuroxime and a three month course of colchicine.
Discussion:
Although our patient endorsed chest pain, he did not demonstrate classic pericarditis signs. Unlike non infectious acute pericarditis, purulent pericarditis typically manifests as fever, tachycardia, and workup that parallels sepsis, highlighting the importance of comprehensive workup. In his case, purulent pericarditis likely resulted from contiguous spread of bacterial pneumonia, the most common route by which streptococcus pneumoniae enters the pericardium. While purulent pericarditis typically affects immunocompromised patients, our immunocompetent patient had recent chest trauma, which likely increased susceptibility by creating a pro inflammatory state. Prompt drainage and antibiotics were essential, as untreated purulent pericarditis mortality is near 100%. Even with correct treatment, mortality can reach up to 30%.
Conclusion:
Even in immunocompetent states, providers should consider purulent pericarditis especially when patients present with sepsis and concerns for pericardial effusion. Early recognition, drainage, and antibiotics are critical to survival.
More abstracts on this topic:
An Inflammatory Dilemma: Human Metapneumovirus-Associated Pericarditis in a Solitary Kidney Host
Rethnaswamy Sherry, King Lauren, Benson Christopher
A Competency-Based Screening Echocardiography Curriculum Designed for Rural American Indian Community Health RepresentativesThoroughman Rose, Riley Alan, De Loizaga Sarah, Adams David, Beaton Andrea, Buonfiglio Samantha, Danforth Kristen, Masyuko Sarah, Miller Mccall, Yadava Mrinal