Final ID: Su3028
Seasonal Variation in New Onset Atrial Fibrillation with Phenotypic Variations in Outcomes, and Projected Trends from a Time Series Analysis
Abstract Body (Do not enter title and authors here): Background: Seasonal variations has been described for new onset atrial fibrillation (NOAF) affecting outcomes. Our study aimed to trend seasonal variation in AF admissions using a nationally representative database, compare in hospital mortality, and identify common comorbid diagnoses linked with NOAF.
Methods: We analyzed the 2016–2022 National Inpatient Sample to identify all non elective hospitalizations for NOAF in adults. Seasons were defined as Winter, Spring, Summer, and Fall. We applied a Seasonal Autoregressive Integrated Moving Average (SARIMA) time-series model to monthly NOAF admissions. Multivariable logistic regression, adjusting for demographic and comorbid factors were estimated for mortality by season, using fall as reference. Top three primary and secondary comorbid diagnoses were identified. We also applied unsupervised Kmeans clustering to reveal distinct seasonal phenotypes on comorbid conditions. P<0.05 was considered statistically significant.
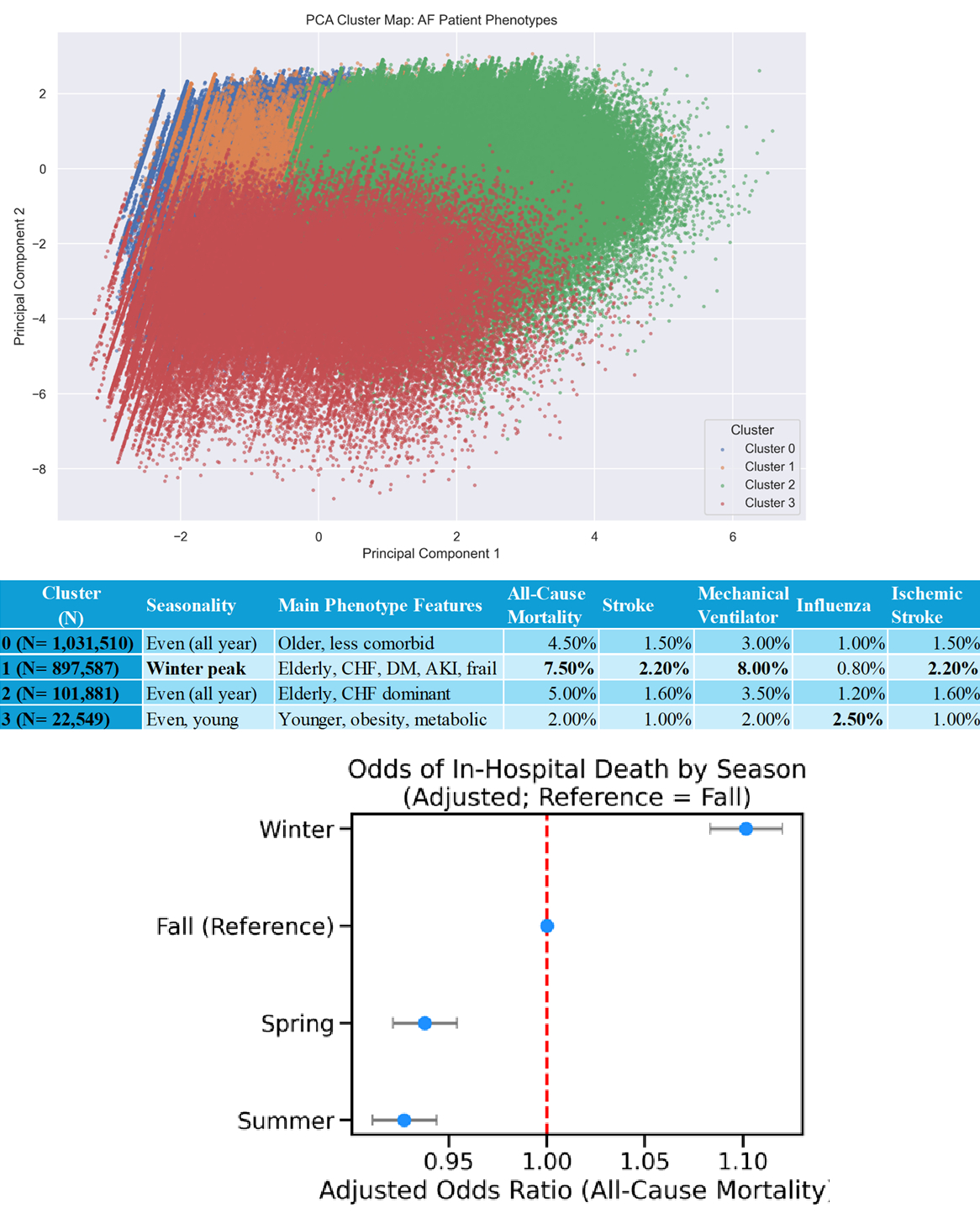
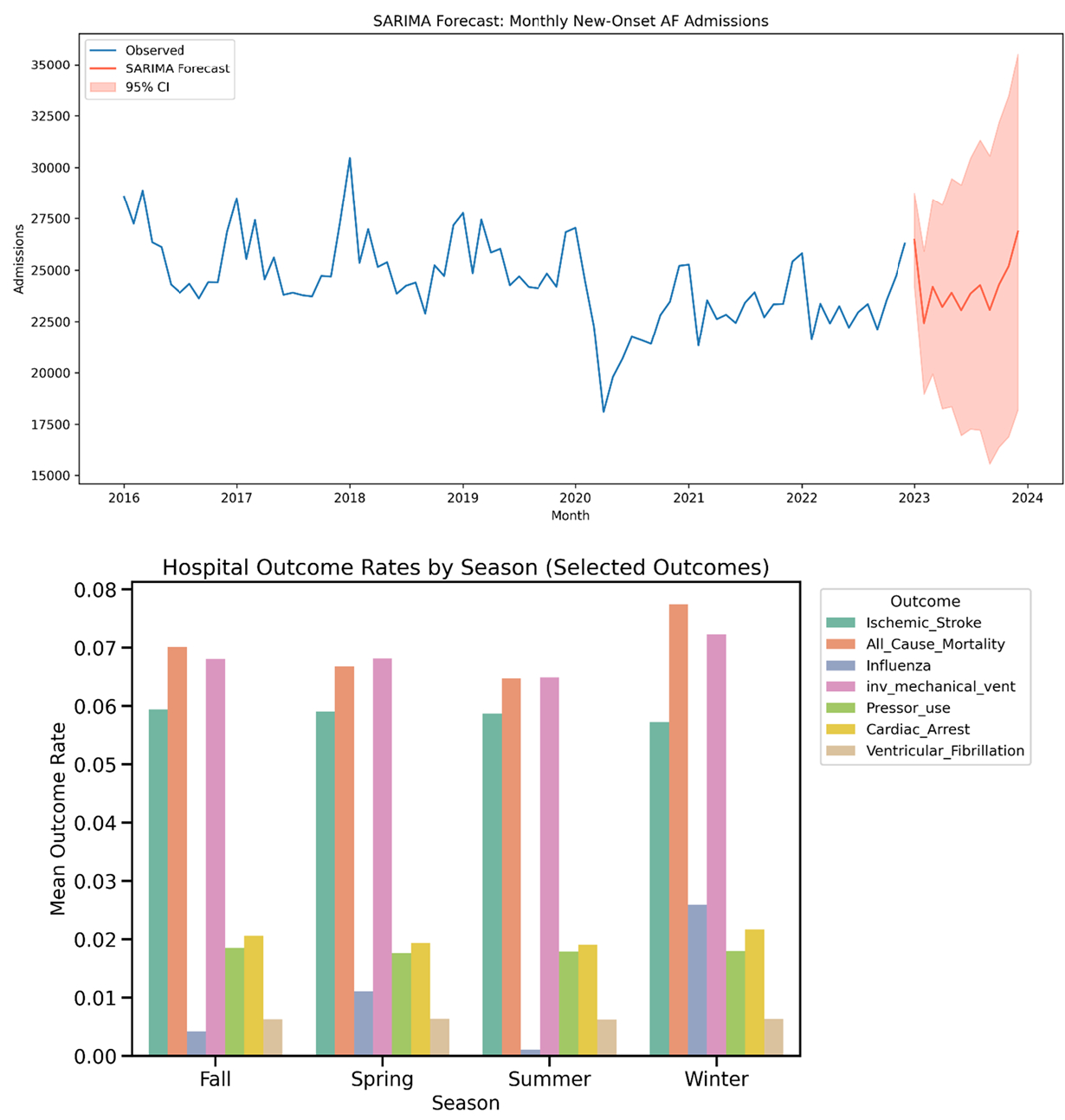
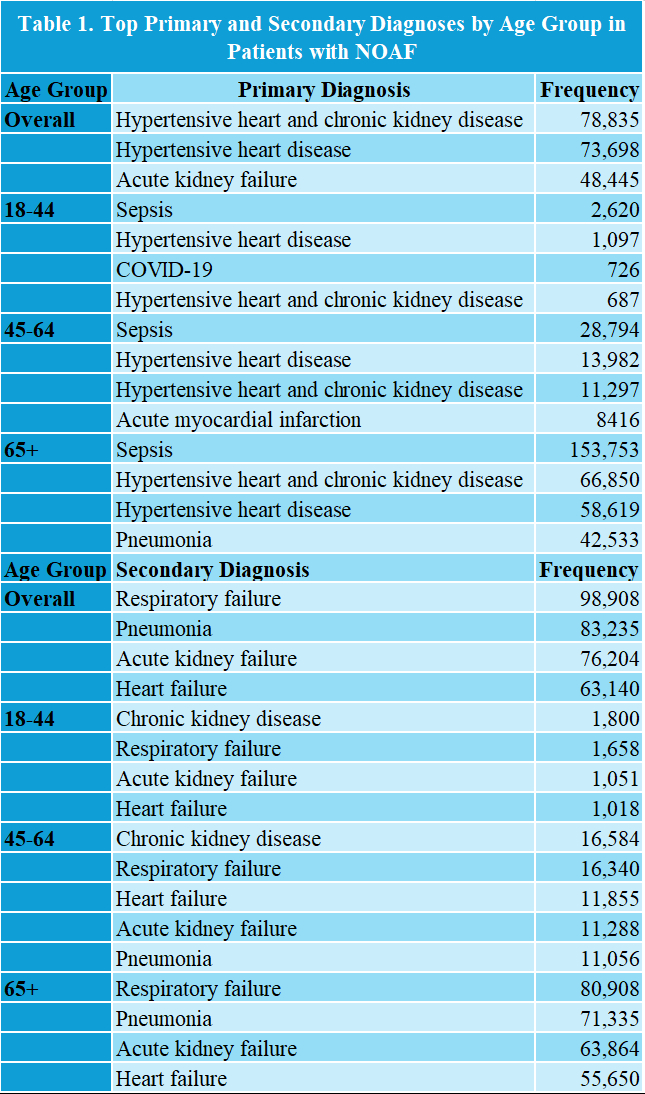
Results: Of total 2,055,000 NOAF admissions, seasonal trend was noted (Winter 555,000; Spring 514,000; Fall 499,000; Summer 492,000), with winter associated with higher odds of in hospital mortality (aOR 1.10; 95% CI 1.08–1.12), whereas spring (aOR 0.97; 95% CI 0.96–0.98; P < 0.001) and summer (aOR 0.93; 95% CI 0.92–0.94; all P < 0.001) had lower odds of death. Unsupervised clustering revealed four distinct phenotypes. Cluster 1 had advanced age, high comorbidity burden, predominance of winter admissions, and demonstrated the highest rates of mortality (7.5%), ischemic stroke (2.2%), and mechanical ventilation (8.0%). In contrast, Cluster 3, composed of younger, more obese patients, showed a higher rate of influenza (2.5%) and lowest mortality (2.0%) (Figure 1). Three most frequent comorbid diagnoses were respiratory failure (4.8%), pneumonia (4.1%), and acute kidney injury (3.7%), and were stratified by age groups (Table 1). The SARIMA model predicted that the monthly number of NOAF will continue to fluctuate with a regular seasonal pattern over the next year, and in-hospital outcomes rates are described by seasons(Figure 2).
Conclusions: NOAF peaked in winter, with highest mortality compared to other seasons. Respiratory failure, pneumonia, and acute kidney failure are the most prevalent comorbid conditions. These findings support need for heightened clinical vigilance, resource allocation, and risk during winter months, in high risk population presenting with NOAF.
Methods: We analyzed the 2016–2022 National Inpatient Sample to identify all non elective hospitalizations for NOAF in adults. Seasons were defined as Winter, Spring, Summer, and Fall. We applied a Seasonal Autoregressive Integrated Moving Average (SARIMA) time-series model to monthly NOAF admissions. Multivariable logistic regression, adjusting for demographic and comorbid factors were estimated for mortality by season, using fall as reference. Top three primary and secondary comorbid diagnoses were identified. We also applied unsupervised Kmeans clustering to reveal distinct seasonal phenotypes on comorbid conditions. P<0.05 was considered statistically significant.
Results: Of total 2,055,000 NOAF admissions, seasonal trend was noted (Winter 555,000; Spring 514,000; Fall 499,000; Summer 492,000), with winter associated with higher odds of in hospital mortality (aOR 1.10; 95% CI 1.08–1.12), whereas spring (aOR 0.97; 95% CI 0.96–0.98; P < 0.001) and summer (aOR 0.93; 95% CI 0.92–0.94; all P < 0.001) had lower odds of death. Unsupervised clustering revealed four distinct phenotypes. Cluster 1 had advanced age, high comorbidity burden, predominance of winter admissions, and demonstrated the highest rates of mortality (7.5%), ischemic stroke (2.2%), and mechanical ventilation (8.0%). In contrast, Cluster 3, composed of younger, more obese patients, showed a higher rate of influenza (2.5%) and lowest mortality (2.0%) (Figure 1). Three most frequent comorbid diagnoses were respiratory failure (4.8%), pneumonia (4.1%), and acute kidney injury (3.7%), and were stratified by age groups (Table 1). The SARIMA model predicted that the monthly number of NOAF will continue to fluctuate with a regular seasonal pattern over the next year, and in-hospital outcomes rates are described by seasons(Figure 2).
Conclusions: NOAF peaked in winter, with highest mortality compared to other seasons. Respiratory failure, pneumonia, and acute kidney failure are the most prevalent comorbid conditions. These findings support need for heightened clinical vigilance, resource allocation, and risk during winter months, in high risk population presenting with NOAF.
More abstracts on this topic:
A novel risk score predicts the prevalence of left atrial low-voltage areas and rhythm outcome in patients undergoing long-standing persistent atrial fibrillation ablation
Ooka Hirotaka, Nakao Sho, Kusuda Masaya, Ariyasu Wataru, Kudo Satoshi, Fujii Subaru, Mano Toshiaki, Matsuda Yasuhiro, Masuda Masaharu, Okamoto Shin, Ishihara Takayuki, Nanto Kiyonori, Tsujimura Takuya, Hata Yosuke, Uematsu Hiroyuki
A Comparison of Outcomes in Heart Failure Patients with and without Iron Deficiency Anemia: A National Database AnalysisBess Olva, Quevedo Ramirez Andres, Shaka Abdultawab, Oredipe Omotola, Bello Jeremiah, Shaka Hafeez