Final ID: MP1063
Pulmonary Hypertension is associated with higher In-Hospital Complications After Transcatheter Mitral Valve Intervention- A Nationwide Analysis of 73,000 Patients
Abstract Body (Do not enter title and authors here): Background Pulmonary hypertension (PH) is commonly associated with mitral valve disease. Transcatheter mitral valve repair (TMVR), involves transseptal approach to replace the diseased mitral valve, but its impact on periprocedural outcomes is not explored in the PHTN group.
Methods We performed a retrospective study of adults undergoing TMVR using the National Inpatient Sample (2016–2022). Patients were stratified by documented PH. Inverse probability of treatment weighting (IPTW) was used on propensity scores (PS). Excellent covariate balance (standardized mean differences(SMD) <10%) and overlap were achieved(Fig 1). Multivariate logistic regression was used to obtain adjusted odds ratios (aORs) for in-hospital primary (all-cause mortality) and secondary outcomes (including stroke, cardiac arrhythmias, acute kidney injury, procedural complications and major adverse cardiovascular events) after adjusting for gender, heart failure, cardiac arrhythmias, diabetes, hypertention prior PCI and CABG for possible confounders based on SMD plot. P<0.05 was considered statistically significant.
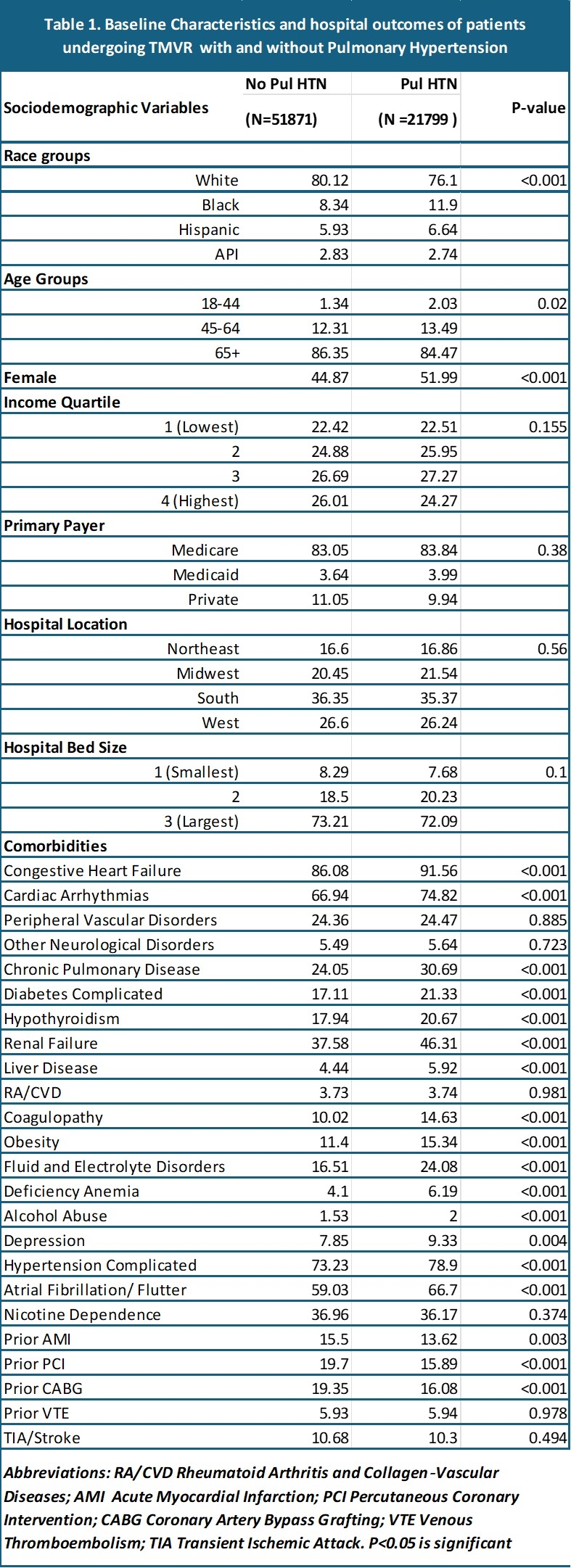
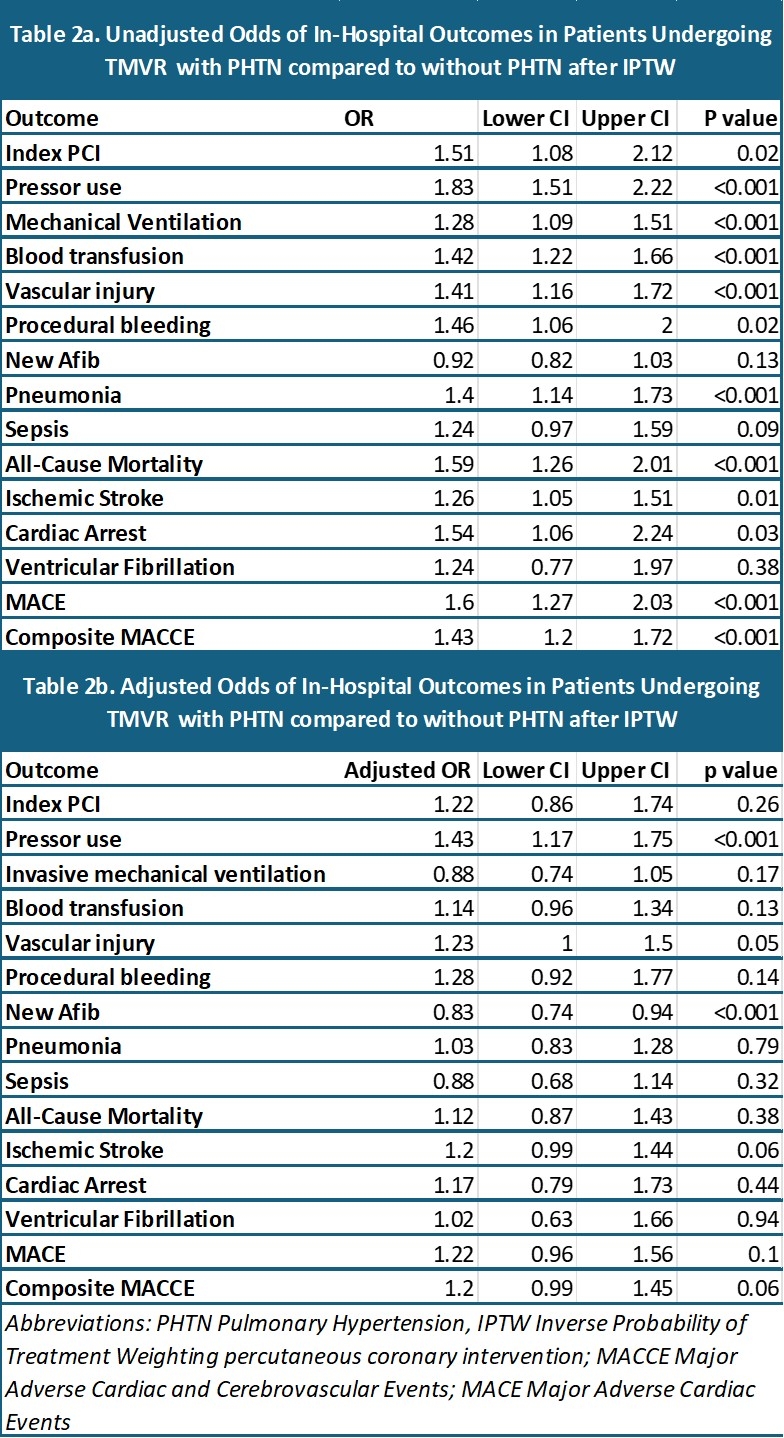
Results Among 73, 670 weighted TMVR admissions (21,799 PH; 51,871 without PH;), the PH cohort more often comprised of females and had higher burden of comorbid conditions (all P<0.05) (Table 1). In unadjusted IPTW analyses, PH was associated with higher odds of index PCI (OR 1.51; 95% CI 1.08–2.12), pressor use (1.83; 1.51–2.22), mechanical ventilation (1.28; 1.09–1.51), blood transfusion (1.42; 1.22–1.66), vascular injury (1.41; 1.16–1.72), procedural bleeding (1.46; 1.06–2.00), pneumonia (1.40; 1.14–1.73), all-cause mortality (1.59; 1.26–2.01), ischemic stroke (1.26; 1.05–1.51), cardiac arrest (1.54; 1.06–2.24), MACE (1.60; 1.27–2.03), and composite MACCE events(1.43; 1.20–1.72) (all p<0.05)(Table 2a). After multivariable adjustment, PH groups had higher odds of pressor use (aOR 1.43; 1.17–1.75; P<0.001),but reduced risk of new atrial fibrillation (0.83; 0.74–0.94; P<0.001).No significant adjusted differences were observed for mortality, MACE, or other complications after adjustment (Table 2b).
Conclusions In TMVR patients, PH predicts greater need for hemodynamic support and is paradoxically linked to lower new onset atrial fibrillation but does not independently increase in hospital mortality or MACE. These findings highlight the importance of optimizing peri procedural management in PH cohorts and curtail worse outcomes in high-risk population groups.
Methods We performed a retrospective study of adults undergoing TMVR using the National Inpatient Sample (2016–2022). Patients were stratified by documented PH. Inverse probability of treatment weighting (IPTW) was used on propensity scores (PS). Excellent covariate balance (standardized mean differences(SMD) <10%) and overlap were achieved(Fig 1). Multivariate logistic regression was used to obtain adjusted odds ratios (aORs) for in-hospital primary (all-cause mortality) and secondary outcomes (including stroke, cardiac arrhythmias, acute kidney injury, procedural complications and major adverse cardiovascular events) after adjusting for gender, heart failure, cardiac arrhythmias, diabetes, hypertention prior PCI and CABG for possible confounders based on SMD plot. P<0.05 was considered statistically significant.
Results Among 73, 670 weighted TMVR admissions (21,799 PH; 51,871 without PH;), the PH cohort more often comprised of females and had higher burden of comorbid conditions (all P<0.05) (Table 1). In unadjusted IPTW analyses, PH was associated with higher odds of index PCI (OR 1.51; 95% CI 1.08–2.12), pressor use (1.83; 1.51–2.22), mechanical ventilation (1.28; 1.09–1.51), blood transfusion (1.42; 1.22–1.66), vascular injury (1.41; 1.16–1.72), procedural bleeding (1.46; 1.06–2.00), pneumonia (1.40; 1.14–1.73), all-cause mortality (1.59; 1.26–2.01), ischemic stroke (1.26; 1.05–1.51), cardiac arrest (1.54; 1.06–2.24), MACE (1.60; 1.27–2.03), and composite MACCE events(1.43; 1.20–1.72) (all p<0.05)(Table 2a). After multivariable adjustment, PH groups had higher odds of pressor use (aOR 1.43; 1.17–1.75; P<0.001),but reduced risk of new atrial fibrillation (0.83; 0.74–0.94; P<0.001).No significant adjusted differences were observed for mortality, MACE, or other complications after adjustment (Table 2b).
Conclusions In TMVR patients, PH predicts greater need for hemodynamic support and is paradoxically linked to lower new onset atrial fibrillation but does not independently increase in hospital mortality or MACE. These findings highlight the importance of optimizing peri procedural management in PH cohorts and curtail worse outcomes in high-risk population groups.
More abstracts on this topic:
Acoramidis Effect on All-Cause Mortality in Patients with p.V142I (V122I) Variant ATTR-CM: Findings From the ATTRibute-CM Study
Alexander Kevin, Bhatt Kunal, Judge Daniel, Grodin Justin, Akinboboye Olakunle, Chen Chris, Tamby Jean-francois, Castano Adam, Fox Jonathan, Fontana Marianna, Gillmore Julian, Sarswat Nitasha, Grogan Martha, Solomon Scott, Davis Margot, Cuddy Sarah, Kittleson Michelle, Shah Keyur, Griffin Jan, Ruberg Frederick, Khouri Michel
A Novel Animal Model for Pulmonary Hypertension: Lung Endothelial Specific Deletion of Egln1 in MiceLiu Bin, Yi Dan, Ramirez Karina, Fallon Michael, Dai Zhiyu