Final ID: Su3094
Troponin Testing Trends in US Emergency Departments
Abstract Body (Do not enter title and authors here): Introduction
Little is known regarding recent temporal trends in troponin testing in US EDs. While insufficient testing risks overlooking MIs, excessive testing may contribute to diagnostic inaccuracies, extended hospitalizations, and unnecessary downstream investigations.
Method
We conducted a pooled cross-sectional analysis of troponin testing trends in US EDs from 1/2019 to 12/2024 using EHRs from Epic Cosmos database which includes more than 290 million patients across the US. ED encounters and corresponding number of patients (≥18 years) were identified. Using reason for visit, tested patients were classified into 3 groups: chest pain (CP), non–chest pain anginal equivalent (NCPAE) (SOB, diaphoresis, nausea, dizziness), and no anginal symptoms. ED diagnosis (1st or 2nd), admitting diagnosis, and/or discharge diagnosis were used to identify ACS. Primary outcome was the proportion of ED visits with troponin testing and subsequent ACS diagnosis. Testing trends over time were analyzed.
Results
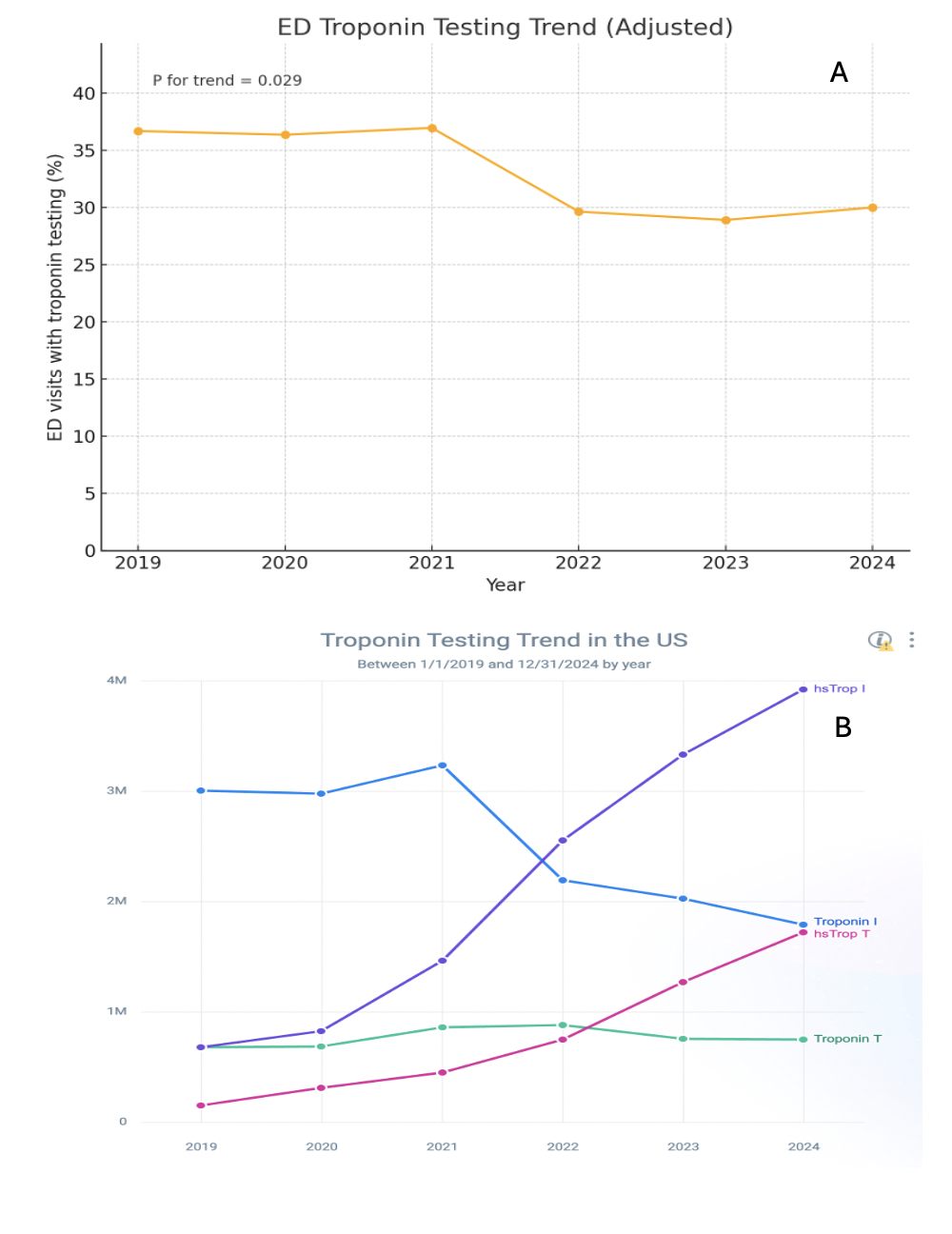
231,544,395 ED encounters accounting for 83,157,740 patients were identified. Among these, 27,514,437 patients (33.1%) underwent quantitative troponin testing. Patients undergoing troponin testing were older (60 ± 20 vs 44 ± 25 yrs), more likely to be female (54.4% vs 51.4%), and white (72.3% vs 67.8%). They had a higher prevalence of HTN (65.0% vs 40.0%), HLD (55.9% vs 34.6%), CKD (20.2% vs 5.0%), and smoking history (10.5% vs 5.3%). Of those tested, 32.8% presented with CP, 20.1% presented with NCPAE, and 47.1% had no anginal symptoms. Abnormal troponin levels were observed in 21.3% of patients (n = 5,860,575; 95% CI: 21.25%–21.35%). A diagnosis of ACS was made in 2.2% of patients who underwent troponin testing (n = 605,166; 95% CI: 2.19%–2.20%). The incidence of ACS was highest in those presenting with CP (3.6%), followed by those with NCPAE (1.12%), and was lowest in patients with nonanginal symptoms (0.84%). On trend analysis, troponin testing rates increased during the COVID-19 pandemic years, followed by a subsequent decline (P trend = 0.03; Fig 1A). From 2019 to 2024, there was a steady decrease in the use of Trop I—and to a lesser extent, Trop T—in favor of hsTroponins (Fig 1B).
Conclusions
Nearly one in three patients presenting to US EDs underwent troponin testing. Among those tested, around one in five patients had abnormal troponins, but only 2.2% were diagnosed with ACS. Refinements in cardiac biomarker testing strategies are needed to optimize ACS diagnosis.
Little is known regarding recent temporal trends in troponin testing in US EDs. While insufficient testing risks overlooking MIs, excessive testing may contribute to diagnostic inaccuracies, extended hospitalizations, and unnecessary downstream investigations.
Method
We conducted a pooled cross-sectional analysis of troponin testing trends in US EDs from 1/2019 to 12/2024 using EHRs from Epic Cosmos database which includes more than 290 million patients across the US. ED encounters and corresponding number of patients (≥18 years) were identified. Using reason for visit, tested patients were classified into 3 groups: chest pain (CP), non–chest pain anginal equivalent (NCPAE) (SOB, diaphoresis, nausea, dizziness), and no anginal symptoms. ED diagnosis (1st or 2nd), admitting diagnosis, and/or discharge diagnosis were used to identify ACS. Primary outcome was the proportion of ED visits with troponin testing and subsequent ACS diagnosis. Testing trends over time were analyzed.
Results
231,544,395 ED encounters accounting for 83,157,740 patients were identified. Among these, 27,514,437 patients (33.1%) underwent quantitative troponin testing. Patients undergoing troponin testing were older (60 ± 20 vs 44 ± 25 yrs), more likely to be female (54.4% vs 51.4%), and white (72.3% vs 67.8%). They had a higher prevalence of HTN (65.0% vs 40.0%), HLD (55.9% vs 34.6%), CKD (20.2% vs 5.0%), and smoking history (10.5% vs 5.3%). Of those tested, 32.8% presented with CP, 20.1% presented with NCPAE, and 47.1% had no anginal symptoms. Abnormal troponin levels were observed in 21.3% of patients (n = 5,860,575; 95% CI: 21.25%–21.35%). A diagnosis of ACS was made in 2.2% of patients who underwent troponin testing (n = 605,166; 95% CI: 2.19%–2.20%). The incidence of ACS was highest in those presenting with CP (3.6%), followed by those with NCPAE (1.12%), and was lowest in patients with nonanginal symptoms (0.84%). On trend analysis, troponin testing rates increased during the COVID-19 pandemic years, followed by a subsequent decline (P trend = 0.03; Fig 1A). From 2019 to 2024, there was a steady decrease in the use of Trop I—and to a lesser extent, Trop T—in favor of hsTroponins (Fig 1B).
Conclusions
Nearly one in three patients presenting to US EDs underwent troponin testing. Among those tested, around one in five patients had abnormal troponins, but only 2.2% were diagnosed with ACS. Refinements in cardiac biomarker testing strategies are needed to optimize ACS diagnosis.
More abstracts on this topic:
Association Between High-Sensitivity Troponin Levels and Hypertension
Karzoun Ahmad, Alkowatli Hamza, Hassan Noheir
Circadian Troponin Dynamics Reveal Sex-Specific Signals for Acute Coronary Syndrome ManagementEmakhu Joshua, Soman Sana, Hawatian Kegham, Cook Bernard, Mccord James, Miller Joseph