Final ID: MP1552
The Effect of the COVID-19 Public Health Emergency on Cardiovascular Care and Cardiac Rehabilitation Access and Use
Abstract Body (Do not enter title and authors here): Background: The COVID-19 Public Health Emergency (PHE) disrupted access to cardiac procedures and cardiac rehabilitation (CR) nationwide. Less is known about the long-term impacts of the PHE on CVD care and CR access and enrollment.
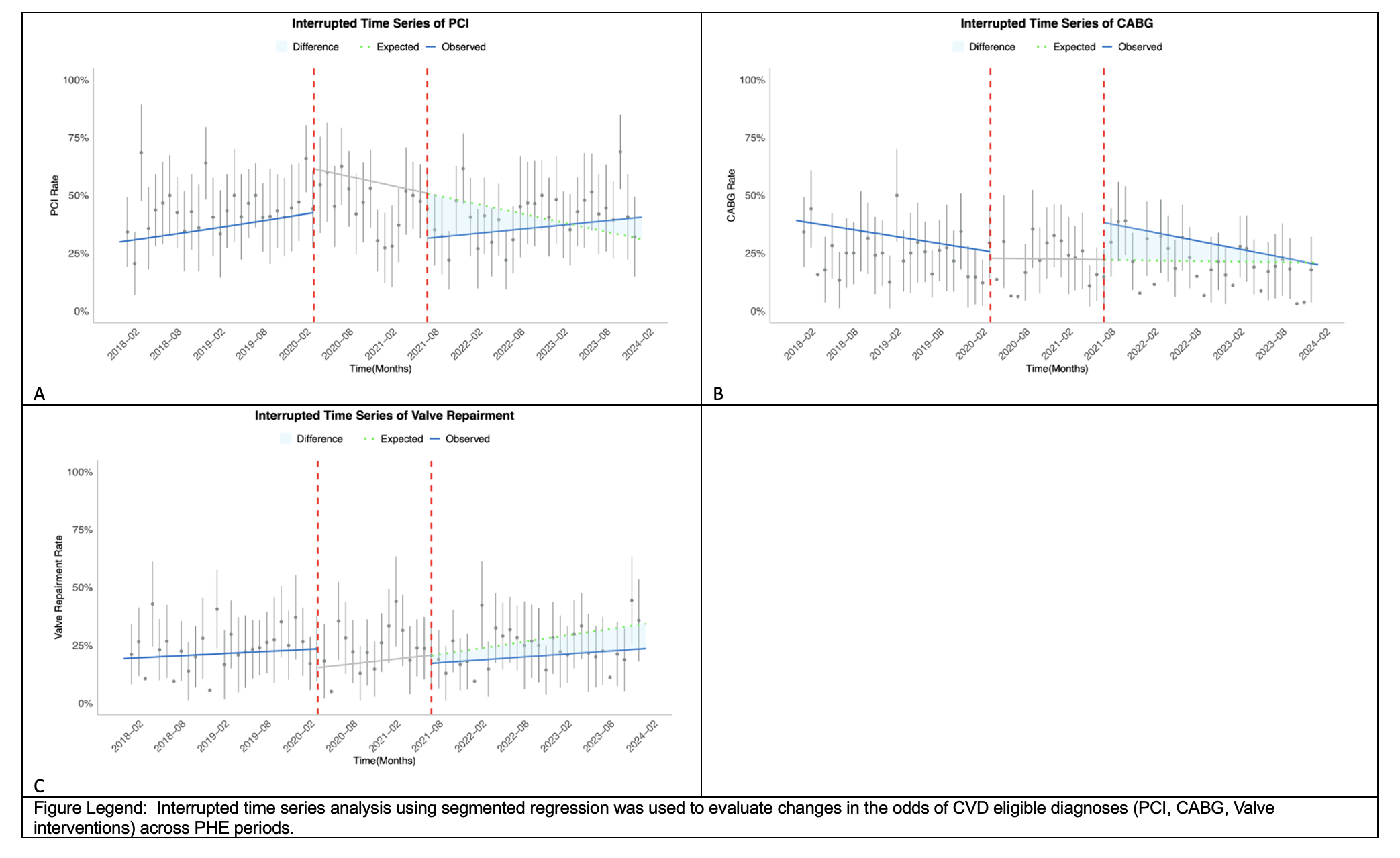
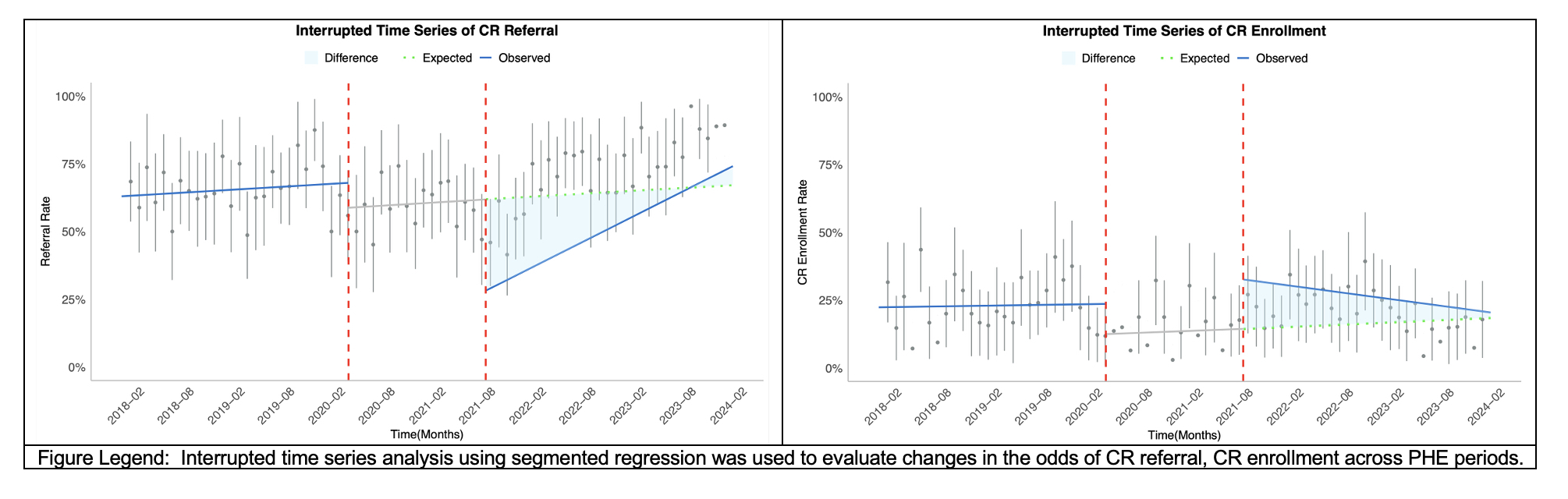
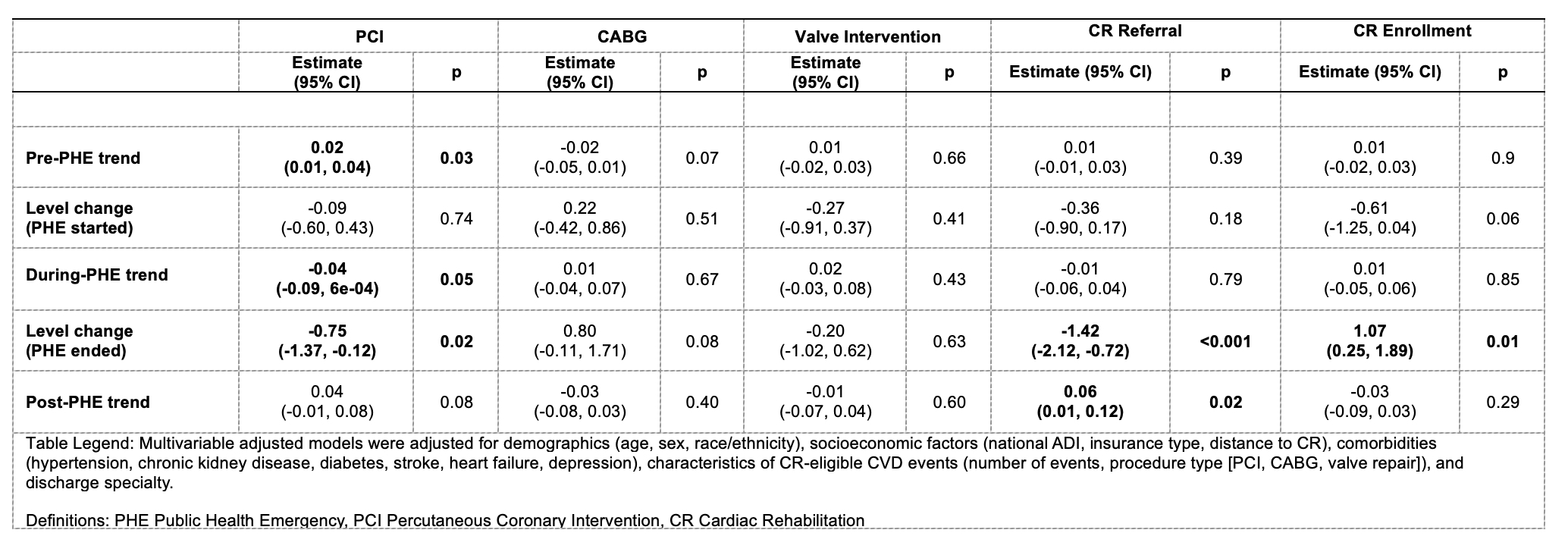
Methods: We used data from a tertiary health system to identify adult patients eligible for CR based on discharge codes for percutaneous coronary intervention (PCI), coronary artery bypass graft surgery (CABG), and valve interventions from January 2018 to December 2023. CR referrals were obtained from electronic orders; CR enrollment was ascertained from billing codes. We analyzed the temporal patterns of cardiac procedures and CR referral and enrollment across three periods: pre-PHE (January 2018-March 2020), during-PHE (March 2020-July 2021), and post-PHE (July 2021-December 2023) using interrupted time series analysis.
Results: There were 2,391 patients eligible for CR, of which 67.2% were referred and 20.5% were enrolled. The mean age was 69.8 (SD 13.1) years, 36.9% women, and 24.2% Black. For PCI, there was an increasing trend pre-PHE (trend 0.02, 95% CI 0.01,0.04) followed by a decline during the PHE with a significantly drop at the end of the PHE (level change: -0.75, 95% CI -1.37 to -0.12) and then a non-significant increasing trend post-PHE. There were non-significant declines in CABG before and after the PHE, while valve interventions were stable. For CR, monthly referral rates were stable at approximately 70% during the pre-PHE period (trend: 0.01, 95% CI -0.01 to 0.03). During the PHE, the referral rate was generally stable and then declined to the lowest point at the end of PHE (level change: -1.42, 95% CI -2.12 to -0.72) (Fig1D). Post-PHE, the referral rates recovered to pre-PHE levels with a significant positive trend (0.06, 95% CI 0.01 to 0.12). Enrollment rates remained stable at approximately 20% pre-PHE and declined to 15% during the PHE. The enrollment rate increased at the end of PHE (level change: 1.07, 95% CI 0.25 to 1.89), followed by a non-significant decreasing trend post-PHE trend (-0.03, 95% CI -0.09 to 0.03) to lower than pre-PHE levels.
Conclusions: There was an increasing trend in PCI use pre-PHE that leveled off during the PHE but has continued to increase post-PHE to pre-PHE levels. In contrast there were non-significant declining trends in CABG while valve interventions remained stable. CR referral has exceeded pre-PHE levels, yet CR enrollment rates have stagnated post-PHE.
Methods: We used data from a tertiary health system to identify adult patients eligible for CR based on discharge codes for percutaneous coronary intervention (PCI), coronary artery bypass graft surgery (CABG), and valve interventions from January 2018 to December 2023. CR referrals were obtained from electronic orders; CR enrollment was ascertained from billing codes. We analyzed the temporal patterns of cardiac procedures and CR referral and enrollment across three periods: pre-PHE (January 2018-March 2020), during-PHE (March 2020-July 2021), and post-PHE (July 2021-December 2023) using interrupted time series analysis.
Results: There were 2,391 patients eligible for CR, of which 67.2% were referred and 20.5% were enrolled. The mean age was 69.8 (SD 13.1) years, 36.9% women, and 24.2% Black. For PCI, there was an increasing trend pre-PHE (trend 0.02, 95% CI 0.01,0.04) followed by a decline during the PHE with a significantly drop at the end of the PHE (level change: -0.75, 95% CI -1.37 to -0.12) and then a non-significant increasing trend post-PHE. There were non-significant declines in CABG before and after the PHE, while valve interventions were stable. For CR, monthly referral rates were stable at approximately 70% during the pre-PHE period (trend: 0.01, 95% CI -0.01 to 0.03). During the PHE, the referral rate was generally stable and then declined to the lowest point at the end of PHE (level change: -1.42, 95% CI -2.12 to -0.72) (Fig1D). Post-PHE, the referral rates recovered to pre-PHE levels with a significant positive trend (0.06, 95% CI 0.01 to 0.12). Enrollment rates remained stable at approximately 20% pre-PHE and declined to 15% during the PHE. The enrollment rate increased at the end of PHE (level change: 1.07, 95% CI 0.25 to 1.89), followed by a non-significant decreasing trend post-PHE trend (-0.03, 95% CI -0.09 to 0.03) to lower than pre-PHE levels.
Conclusions: There was an increasing trend in PCI use pre-PHE that leveled off during the PHE but has continued to increase post-PHE to pre-PHE levels. In contrast there were non-significant declining trends in CABG while valve interventions remained stable. CR referral has exceeded pre-PHE levels, yet CR enrollment rates have stagnated post-PHE.
More abstracts on this topic:
Assessing the Impact of a Healthy Foods Center Program Has on Food Insecurity and Healthcare Outcomes: A Pilot Study
Drury-gworek Charlotte, Galper Kathleen, Barrett Tyson, Shergill Amber, Cuevas Elizabeth, Ereditario Colleen
Association of heat exposure with cardiovascular and all-cause hospitalizations among elderly adults in the United StatesBansal Esha, Puvvula Jagadeesh, Shultz Kaitlyn, Khatana Sameed Ahmed