Final ID: MP1920
Calcitonin Gene-Related Peptide (CGRP) Inhibitor Use Is Associated With Increased Cardiovascular Event Risk in Patients with Migraine: A Nationwide Study
Abstract Body (Do not enter title and authors here):
Introduction: Calcitonin gene-related peptide (CGRP) inhibitors are increasingly used in the United States (US) for the prevention and treatment of migraine, but population-based data on their cardiovascular risk profile are lacking.
Research Objective/Aims: To evaluate the association between CGRP inhibitor initiation and cardiovascular events.
Methods. This was a retrospective, observational, cohort study using claims data from a proprietary, insurance-based registry – Marketscan (by Merative). Beneficiaries with at least one migraine-related claim and continuous coverage for at least 12 months prior to migraine diagnosis were included. Using a sequential trial framework, the rate of cardiovascular events was computed in those who did and did not initiate a CGRP inhibitor, using both crude estimates and those derived in propensity score-overlap weighted cohorts. The primary end point was a composite of myocardial infarction, cerebral ischemic stroke, revascularization, the development of peripheral arterial disease, or central retinal artery occlusion. Secondary end points included each component of the composite end point individually. A falsification end point (humeral fracture) was included. Adjusted hazard ratios (HR) and corresponding 95% confidence intervals (CI) were computed.
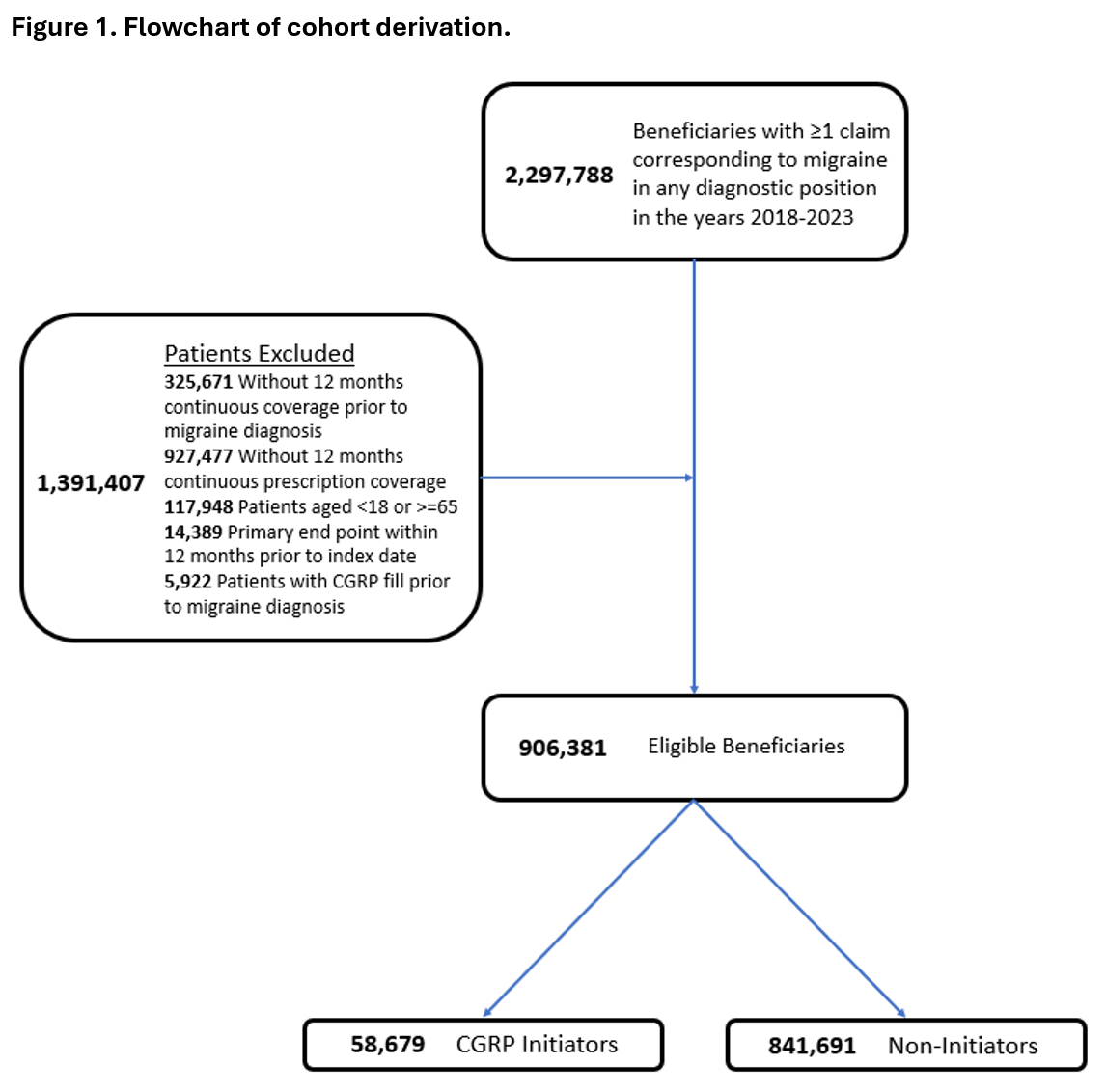
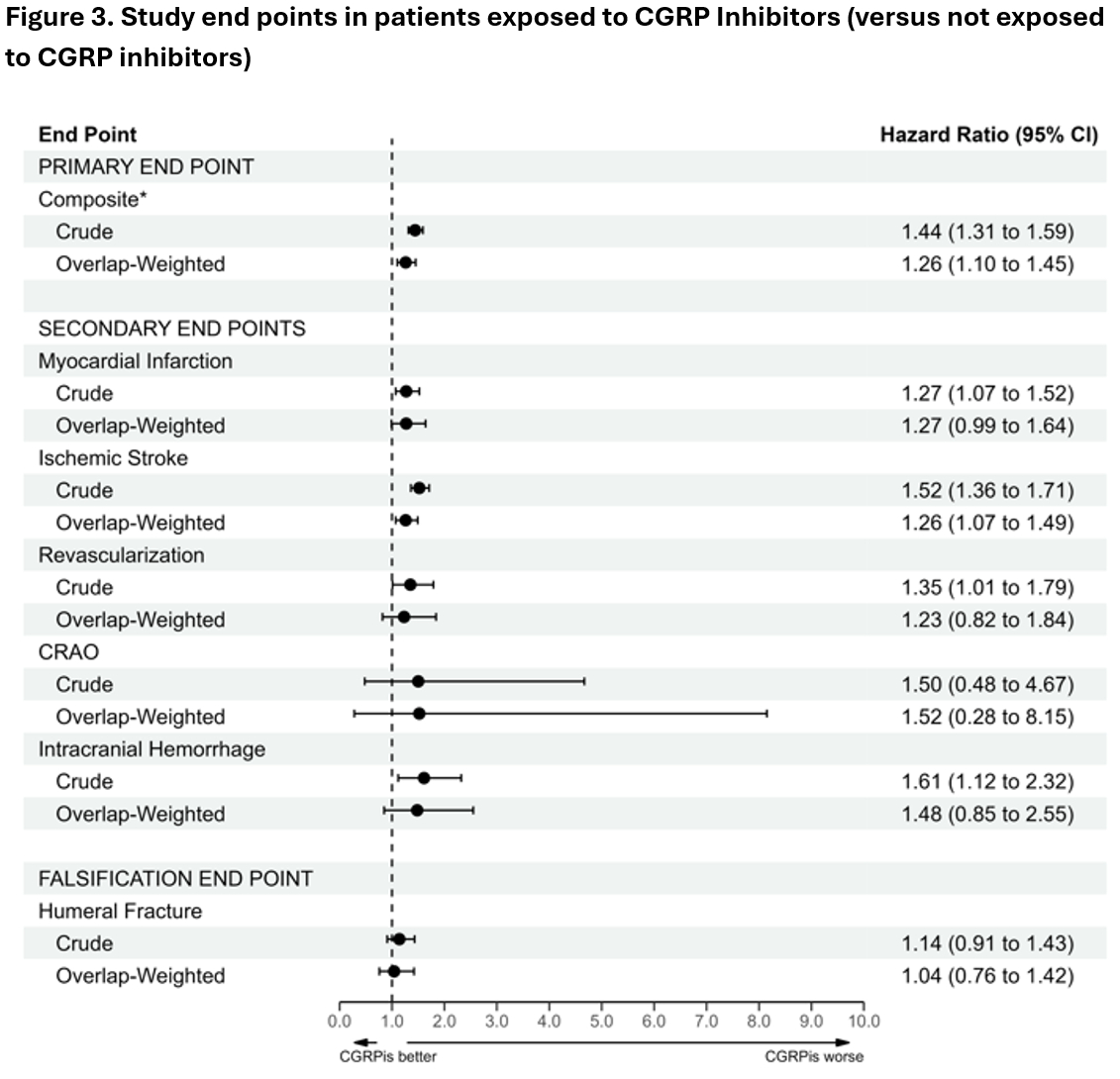
Results: In total, 900,370 beneficiaries (median age 41 [Q1, Q3: 31, 51]; 77.8% female) were included of whom 58,679 initiated a CGRP inhibitor and 841,691 did not initiate a CGRP inhibitor during the study period. The derivation of the study population is shown in Figure 1. Characteristics of the included patients by CGRP use status are shown in Figure 2. In the propensity score overlap-weighted analysis, there was a higher rate of the primary end point in beneficiaries who initiated a CGRP inhibitor (8.77 events/1,000 person-years vs. 6.76 events/1,000 person-years; aHR 1.26 [95% CI: 1.10 – 1.45]). Initiation of a CGRP inhibitor was associated with a significantly higher rate of one secondary end point (ischemic stroke [aHR 1.26 (95% CI: 1.07 – 1.49)]) but not 4 other secondary end points: MI, revascularization, CRAO, and ICH. Overall results of primary and secondary endpoints are summarized in Figure 3.
Conclusions: In a population-based cohort study, initiation of a CGRP inhibitor was associated with an increased risk of a composite of cardiovascular events, however the magnitude of the increased risk was low and results are vulnerable to residual, unmeasured confounding.
Introduction: Calcitonin gene-related peptide (CGRP) inhibitors are increasingly used in the United States (US) for the prevention and treatment of migraine, but population-based data on their cardiovascular risk profile are lacking.
Research Objective/Aims: To evaluate the association between CGRP inhibitor initiation and cardiovascular events.
Methods. This was a retrospective, observational, cohort study using claims data from a proprietary, insurance-based registry – Marketscan (by Merative). Beneficiaries with at least one migraine-related claim and continuous coverage for at least 12 months prior to migraine diagnosis were included. Using a sequential trial framework, the rate of cardiovascular events was computed in those who did and did not initiate a CGRP inhibitor, using both crude estimates and those derived in propensity score-overlap weighted cohorts. The primary end point was a composite of myocardial infarction, cerebral ischemic stroke, revascularization, the development of peripheral arterial disease, or central retinal artery occlusion. Secondary end points included each component of the composite end point individually. A falsification end point (humeral fracture) was included. Adjusted hazard ratios (HR) and corresponding 95% confidence intervals (CI) were computed.
Results: In total, 900,370 beneficiaries (median age 41 [Q1, Q3: 31, 51]; 77.8% female) were included of whom 58,679 initiated a CGRP inhibitor and 841,691 did not initiate a CGRP inhibitor during the study period. The derivation of the study population is shown in Figure 1. Characteristics of the included patients by CGRP use status are shown in Figure 2. In the propensity score overlap-weighted analysis, there was a higher rate of the primary end point in beneficiaries who initiated a CGRP inhibitor (8.77 events/1,000 person-years vs. 6.76 events/1,000 person-years; aHR 1.26 [95% CI: 1.10 – 1.45]). Initiation of a CGRP inhibitor was associated with a significantly higher rate of one secondary end point (ischemic stroke [aHR 1.26 (95% CI: 1.07 – 1.49)]) but not 4 other secondary end points: MI, revascularization, CRAO, and ICH. Overall results of primary and secondary endpoints are summarized in Figure 3.
Conclusions: In a population-based cohort study, initiation of a CGRP inhibitor was associated with an increased risk of a composite of cardiovascular events, however the magnitude of the increased risk was low and results are vulnerable to residual, unmeasured confounding.
More abstracts on this topic:
Accuracy Of Stroke Prediction Using The Predicting Risk Of CVD Events Equation Among Diverse Adults Of The Northern Manhattan Study
Mesa Robert, Veledar Emir, Levin Bonnie, Agudelo Christian, Elfassy Tali, Gardener Hannah, Rundek Tatjana, Brown Scott, Yang Eugene, Elkind Mitchell, Gutierrez Jose, Besser Lilah, Gutierrez Carolina
A Contactless and Automated Approach to the Acute Stroke AssessmentSaadat Moh, Titus Ryan, Verkuilen Haley, Fleming Phil, Sur Sanjib, Sen Souvik