Final ID: 4367343
Transgender Male and Gender Non-Binary/Genderqueer Patients are Less Likely to Receive Guideline-Indicated Cardiovascular Care than Cisgender Patients: A Nationwide Study
Abstract Body (Do not enter title and authors here):
Introduction: People identifying as transgender, non-binary, or genderqueer are at higher risk for cardiovascular disease. Additionally, bias and overt discrimination limit care access and could impact care quality for this patient population.
Research Question/Aims: To understand whether disparities in cardiovascular care quality exist for patients who identify as transgender or non-binary/genderqueer in routine clinical practice.
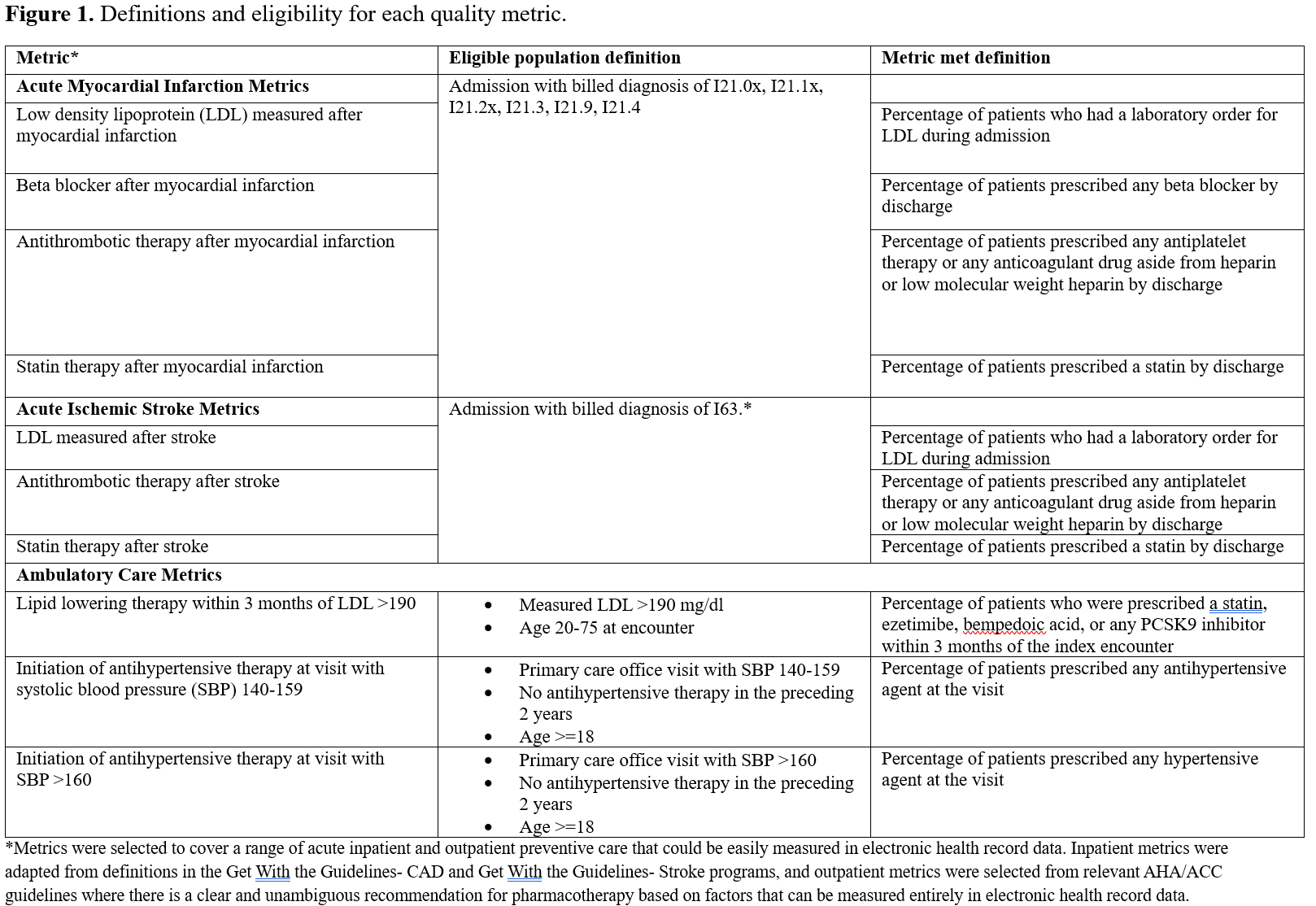
Methods: We used data from Epic Cosmos, a dataset of Epic Health systems representing more than 300 million patient records, from January 1, 2021-December 31, 2024. Epic Cosmos collects harmonized patient gender identity information from participating health systems, with completion rates between 14-20% during the study period. Gender identity was classified as follows: cisgender male, cisgender female, transgender male, transgender female, gender non-binary/genderqueer (inclusive of gender non-binary, other gender, or genderqueer, which were grouped due to low sample size), and choose not to respond. Rates of achievement of key cardiovascular care quality metrics were calculated for patients of each gender identity group. Figure 1 details the criteria for eligibility and achievement of each care quality metric. Rate ratios and 95% confidence intervals were calculated with a reference group of cisgender male for transgender male patients, cisgender female for transgender female patients, and cisgender (male or female) for gender non-binary/genderqueer patients.
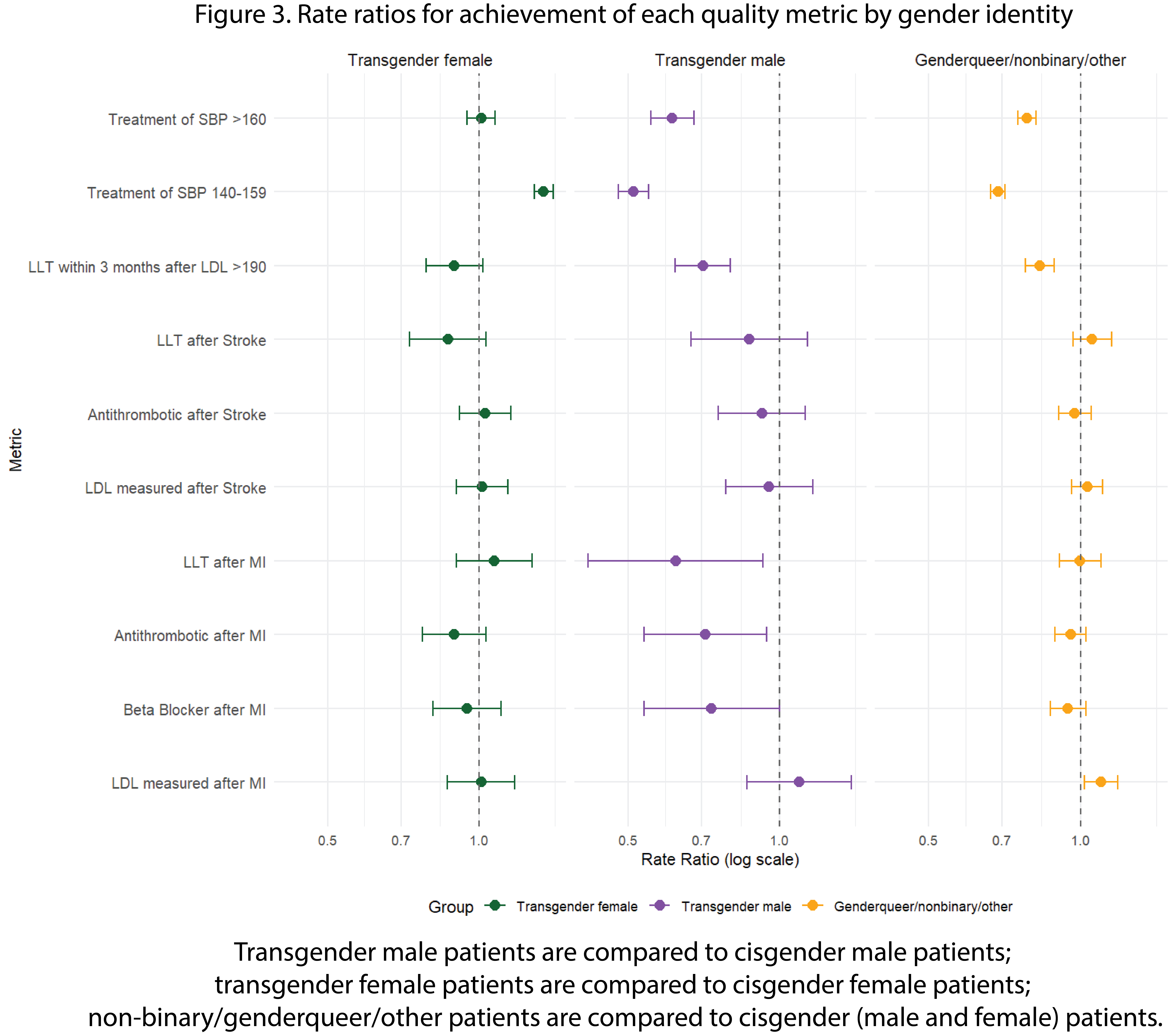
Results: Figure 2 shows the number of eligible patients and number of patients meeting criteria for each quality metric by gender identity. Figure 3 summarizes the rate ratios of metric achievement for each group. In summary, patients identifying as genderqueer/non-binary were less likely to receive lipid lowering therapy after a measured LDL >190 and were less likely to have SBP 140-159 or SBP >160 treated. Transgender male patients were less likely to receive beta blocker, statin, or antithrombotic therapy after acute myocardial infarction, and were less likely to have LDL >190 treated or to have SBP 140-159 or SBP >160 treated.
Conclusions: Transgender male and non-binary/genderqueer patients appear to be less likely to receive some guideline-indicated cardiovascular care. Quality improvement programs should pay attention to these particularly high-risk patient populations to promote equitable delivery of cardiovascular care.
Introduction: People identifying as transgender, non-binary, or genderqueer are at higher risk for cardiovascular disease. Additionally, bias and overt discrimination limit care access and could impact care quality for this patient population.
Research Question/Aims: To understand whether disparities in cardiovascular care quality exist for patients who identify as transgender or non-binary/genderqueer in routine clinical practice.
Methods: We used data from Epic Cosmos, a dataset of Epic Health systems representing more than 300 million patient records, from January 1, 2021-December 31, 2024. Epic Cosmos collects harmonized patient gender identity information from participating health systems, with completion rates between 14-20% during the study period. Gender identity was classified as follows: cisgender male, cisgender female, transgender male, transgender female, gender non-binary/genderqueer (inclusive of gender non-binary, other gender, or genderqueer, which were grouped due to low sample size), and choose not to respond. Rates of achievement of key cardiovascular care quality metrics were calculated for patients of each gender identity group. Figure 1 details the criteria for eligibility and achievement of each care quality metric. Rate ratios and 95% confidence intervals were calculated with a reference group of cisgender male for transgender male patients, cisgender female for transgender female patients, and cisgender (male or female) for gender non-binary/genderqueer patients.
Results: Figure 2 shows the number of eligible patients and number of patients meeting criteria for each quality metric by gender identity. Figure 3 summarizes the rate ratios of metric achievement for each group. In summary, patients identifying as genderqueer/non-binary were less likely to receive lipid lowering therapy after a measured LDL >190 and were less likely to have SBP 140-159 or SBP >160 treated. Transgender male patients were less likely to receive beta blocker, statin, or antithrombotic therapy after acute myocardial infarction, and were less likely to have LDL >190 treated or to have SBP 140-159 or SBP >160 treated.
Conclusions: Transgender male and non-binary/genderqueer patients appear to be less likely to receive some guideline-indicated cardiovascular care. Quality improvement programs should pay attention to these particularly high-risk patient populations to promote equitable delivery of cardiovascular care.
More abstracts on this topic:
D-dimer as a 5-year predictor of death in females admitted with chestpain of suspected coronary origin surpasses that of males.
Nilsen Dennis, Brugger-andersen Trygve, Aarsetoey Reidun, Ueland Thor, Michelsen Annika, Aukrust Pal, Poenitz Volker, Staines Harry, Grundt Heidi
Cocaine Use, Hypertensive Emergency, and Aortic Dissection: A Nationwide Trend and Outcome Analysis from 2016–2021Philip Anil, George Lina James, Saha Shubhashis, Caputi Zuniga Angelo, John Kevin, Nayar Jemimah, Mautong Hans, Odoi Samuel