Final ID: MP2189
Among Older Adults With Atrial Fibrillation, First Anticoagulant Prescription Is Not Associated with Reduced Hazard of Ischemic Stroke but Is Associated with Increased Hazard of Major Bleeding: A Nationwide Study
Abstract Body (Do not enter title and authors here):
Introduction: Sevferal trials have demonstrated that oral anticoagulation reduces ischemic stroke risk in patients with atrial fibrillation (AF), the most common cardiac arrythmia among older adults. The impact of initiation of an anticoagulant on ischemic stroke risk in real-world clinical practice is not known.
Research Objective/Aim: To determine the association between initiation of anticoagulation and the hazard of ischemic stroke and major bleeding events among older adults with incident AF.
Methods: This was a retrospective cohort study based on inpatient, outpatient, emergency department, and skilled nursing facility claims files for a 5% sample of United States fee-for-service Medicare beneficiaries aged 66 years and older who developed incident AF between 2007 and 2020. Using a sequential trial framework, the rates of ischemic stroke and major bleeding events were computed in those who did and did not initiate an anticoagulant, using both crude estimates and those derived in propensity score-overlap weighted cohorts. The primary effectiveness endpoint was ischemic stroke. The primary safety end point was major bleeding. To reduce the impact of selection bias and immortal time bias, unadjusted and adjusted hazard ratios (HRs) and rate differences were computed in a dataset comprised of pooled, sequential clinical trial replicates starting one month apart.
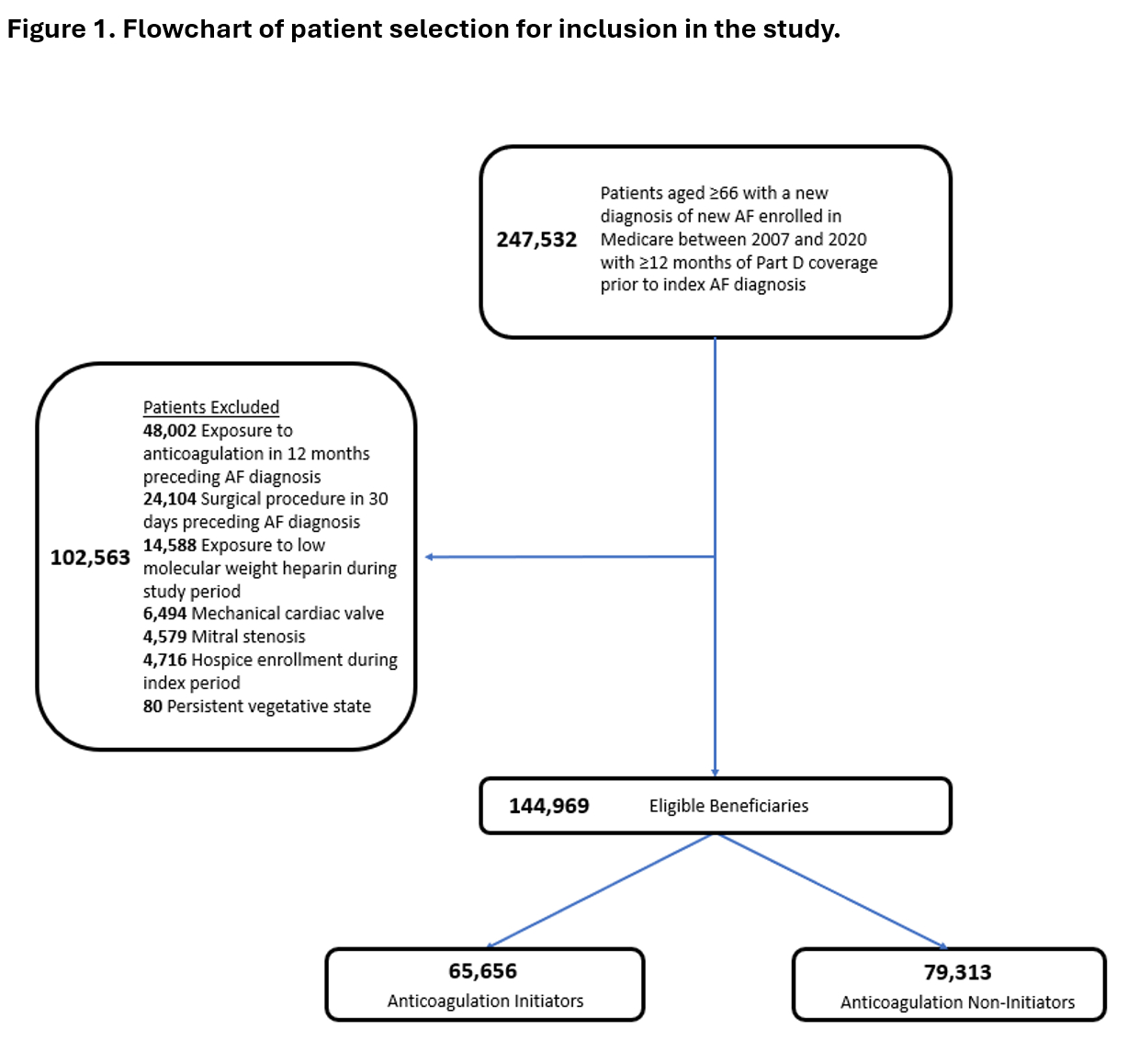
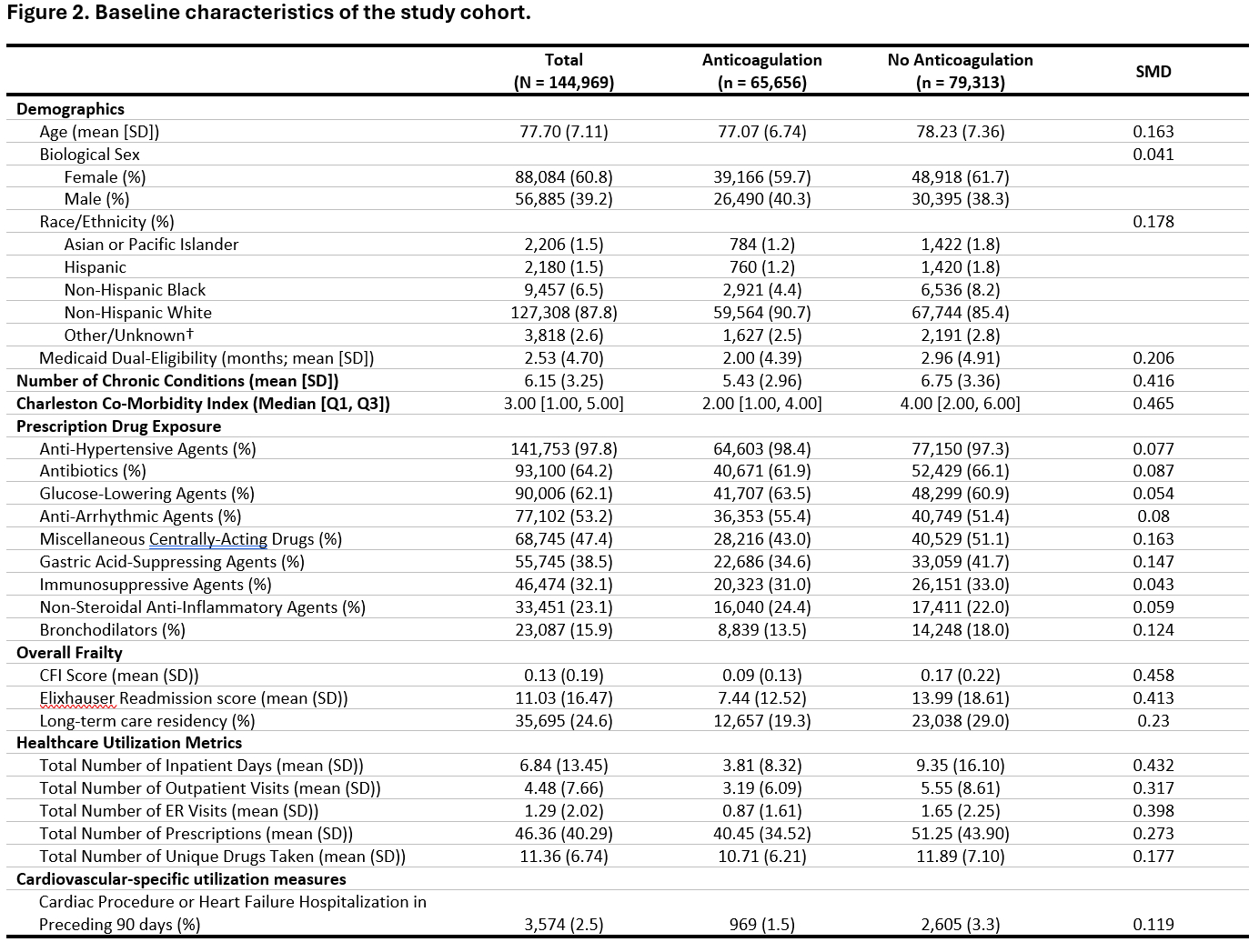
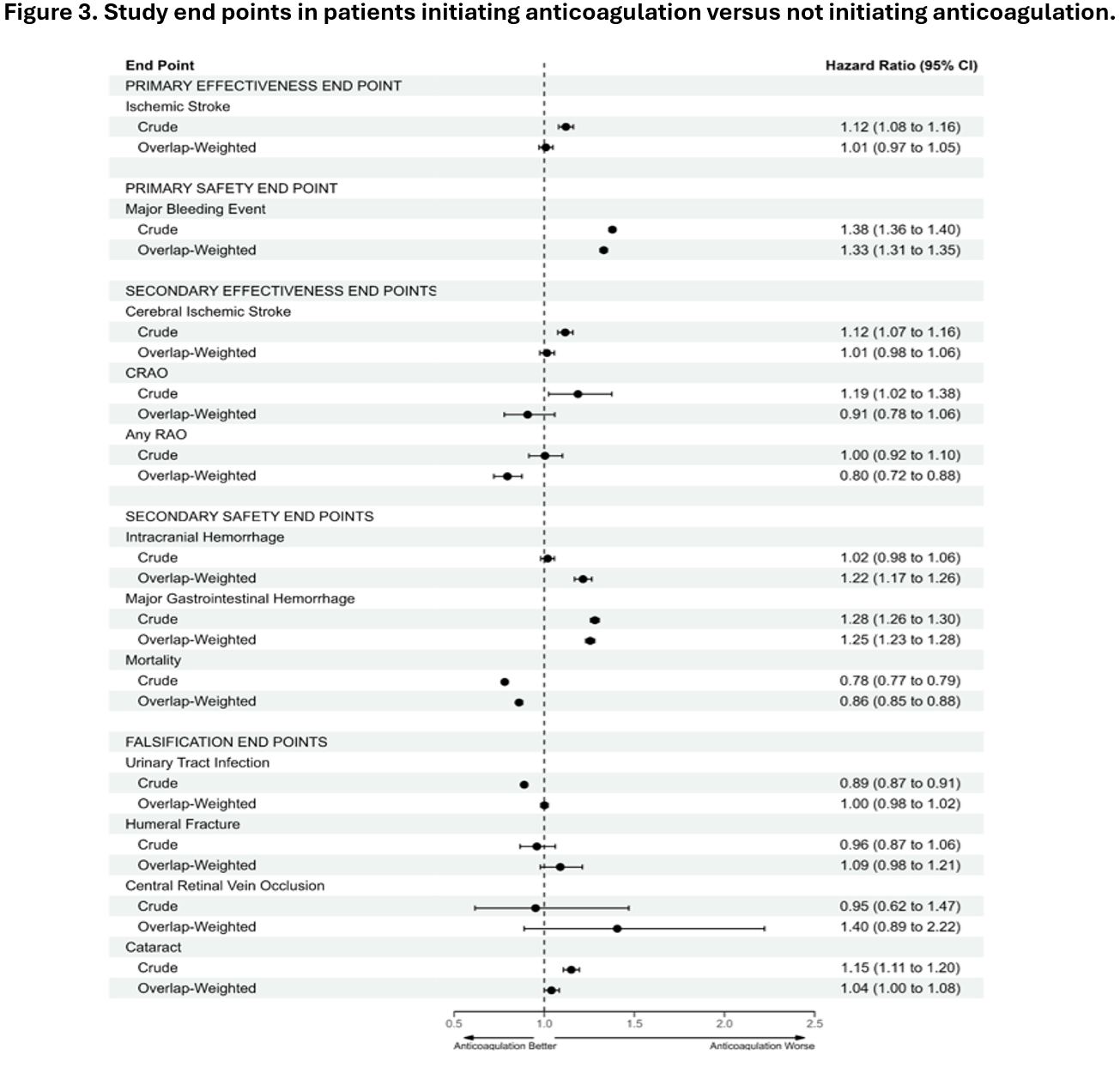
Results: In total, 144,969 patients (60.8% female; mean age 77.7 years [standard deviation (SD) 7.1]) were included in the study. Figure 1 shows the flowchart of patient selection. Figure 2 shows the characteristics of the cohort. Figure 3 summarizes study end points. The mean follow-up period was 3.46 years (SD 2.98 years). Initiation of anticoagulation was not associated with a reduced hazard of ischemic stroke (adjusted hazard ratio [aHR] 1.01 [95% CI: 0.97 – 1.05]). However, initiation of anticoagulation was associated with an increased hazard of a major bleeding event (aHR 1.38 [95% CI: 1.36 – 1.40]) and increased hazards of intracerebral hemorrhage (ICH), and major gastrointestinal hemorrhage. There was a reduced hazard of all-cause mortality (aHR 0.86 [95% CI: 0.85 – 0.88]) and no difference in the hazard of 4 falsification end points.
Conclusion: Among older adults, first anticoagulant prescription was not associated with a reduced hazard of ischemic stroke. However, crude analyses suggested that clinicians are appropriately selecting patients for anticoagulation in routine clinical practice.
Introduction: Sevferal trials have demonstrated that oral anticoagulation reduces ischemic stroke risk in patients with atrial fibrillation (AF), the most common cardiac arrythmia among older adults. The impact of initiation of an anticoagulant on ischemic stroke risk in real-world clinical practice is not known.
Research Objective/Aim: To determine the association between initiation of anticoagulation and the hazard of ischemic stroke and major bleeding events among older adults with incident AF.
Methods: This was a retrospective cohort study based on inpatient, outpatient, emergency department, and skilled nursing facility claims files for a 5% sample of United States fee-for-service Medicare beneficiaries aged 66 years and older who developed incident AF between 2007 and 2020. Using a sequential trial framework, the rates of ischemic stroke and major bleeding events were computed in those who did and did not initiate an anticoagulant, using both crude estimates and those derived in propensity score-overlap weighted cohorts. The primary effectiveness endpoint was ischemic stroke. The primary safety end point was major bleeding. To reduce the impact of selection bias and immortal time bias, unadjusted and adjusted hazard ratios (HRs) and rate differences were computed in a dataset comprised of pooled, sequential clinical trial replicates starting one month apart.
Results: In total, 144,969 patients (60.8% female; mean age 77.7 years [standard deviation (SD) 7.1]) were included in the study. Figure 1 shows the flowchart of patient selection. Figure 2 shows the characteristics of the cohort. Figure 3 summarizes study end points. The mean follow-up period was 3.46 years (SD 2.98 years). Initiation of anticoagulation was not associated with a reduced hazard of ischemic stroke (adjusted hazard ratio [aHR] 1.01 [95% CI: 0.97 – 1.05]). However, initiation of anticoagulation was associated with an increased hazard of a major bleeding event (aHR 1.38 [95% CI: 1.36 – 1.40]) and increased hazards of intracerebral hemorrhage (ICH), and major gastrointestinal hemorrhage. There was a reduced hazard of all-cause mortality (aHR 0.86 [95% CI: 0.85 – 0.88]) and no difference in the hazard of 4 falsification end points.
Conclusion: Among older adults, first anticoagulant prescription was not associated with a reduced hazard of ischemic stroke. However, crude analyses suggested that clinicians are appropriately selecting patients for anticoagulation in routine clinical practice.
More abstracts on this topic:
Anticoagulation versus Antiplatelets in Coronary Artery Ectasia and Acute Coronary Syndrome: A Systematic Review and Meta-analysis
Hernandez-pastrana Sarai, Latapi Ruiz Esparza Ximena, Martignoni Felipe, Araiza Diego, Doma Mohamed, Fatima Syeda Rubab, Hemdanieh Maya, Kritya Mangesh, Huang Wilbert, Naji Zahra, Lingamsetty Shanmukh Sai Pavan, Gewehr Douglas
10-Year Trend Analysis of Medicare Payment in Stroke Inpatient Hospital AdmissionWong Ka-ho, Krothapalli Neeharika, Littig Lauren, Champagne Alison, Majersik Jennifer, Reddy Vivek, De Havenon Adam