Final ID: Mo2097
Cognitive-Behavioral Therapy for Undiagnosed OCD Dramatically Improves Medication Adherence in a Treatment-Resistant Hypertension Patient: A Case Report
Abstract Body (Do not enter title and authors here): Introduction
Resistant hypertension, defined as blood pressure uncontrolled despite optimal use of three or more antihypertensives, is often attributed to physiological causes. However, nonadherence—frequently driven by psychological factors—remains under-recognized. Emerging evidence suggests that untreated psychiatric comorbidities, including obsessive-compulsive disorder (OCD), can drive medication nonadherence through ritualistic behaviors or irrational fears. Cognitive-behavioral therapy (CBT), particularly Exposure and Response Prevention (ERP), is a first-line intervention for OCD and has shown benefit in improving adherence. This case illustrates how targeted ERP for undiagnosed OCD in a patient with presumed treatment-resistant hypertension led to dramatic improvements in both adherence and blood pressure control.
Case Description
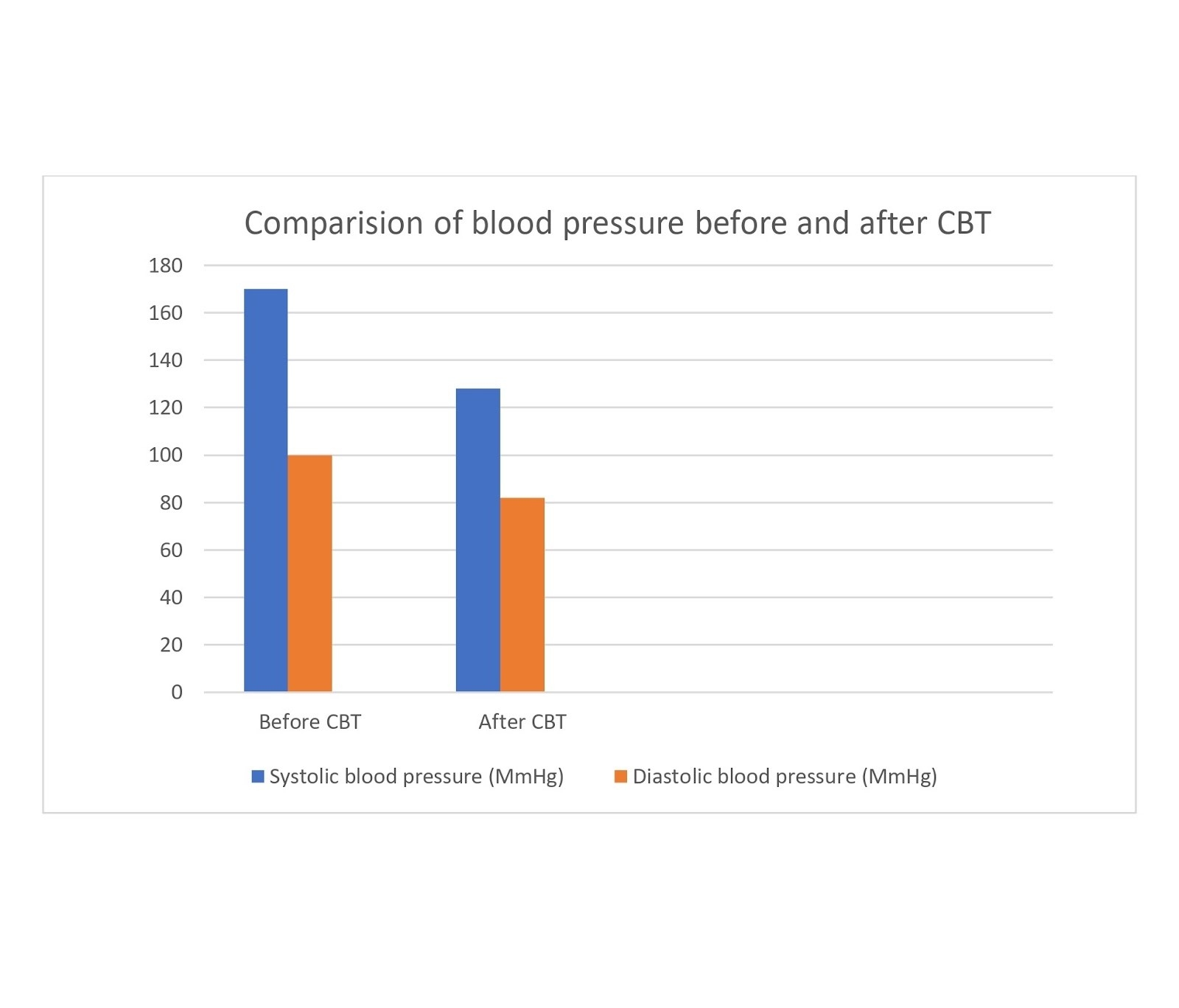
A 52-year-old male with long-standing hypertension (BP 170/100 mmHg) presented repeatedly to the ED despite being on triple antihypertensive therapy. The patient reported anxiety surrounding medication side effects, and disclosed compulsive pill-counting, hoarding, and dose-skipping behaviors, especially if routines were disrupted. Psychiatric evaluation revealed previously undiagnosed OCD (Y-BOCS score 28), primarily centered on contamination fears. He underwent 12 weeks of structured ERP therapy focusing on medication-related rituals. Following treatment, his BP decreased to 128/82 mmHg, and medication adherence improved to 100%, confirmed through pill counts and electronic monitors. Emergency room visits dropped from six per year to zero.
Discussion
This case underscores how OCD can present as “compulsive non-adherence,” where rituals—rather than deliberate refusal—drive treatment failure. Traditional adherence strategies (education, reminders) would likely have failed in this case. Instead, ERP successfully disrupted the OCD cycle, resolving the core behavioral barrier to adherence. This case reframes nonadherence not as defiance but as a psychiatric symptom, demanding psychiatric solutions. It advocates for routine mental health screening in patients with apparent treatment-resistant conditions and highlights the critical role of behavioral cardiology in managing chronic disease. Recognizing psychological drivers of nonadherence can lead to transformative improvements in both physiological outcomes and quality of life.
Resistant hypertension, defined as blood pressure uncontrolled despite optimal use of three or more antihypertensives, is often attributed to physiological causes. However, nonadherence—frequently driven by psychological factors—remains under-recognized. Emerging evidence suggests that untreated psychiatric comorbidities, including obsessive-compulsive disorder (OCD), can drive medication nonadherence through ritualistic behaviors or irrational fears. Cognitive-behavioral therapy (CBT), particularly Exposure and Response Prevention (ERP), is a first-line intervention for OCD and has shown benefit in improving adherence. This case illustrates how targeted ERP for undiagnosed OCD in a patient with presumed treatment-resistant hypertension led to dramatic improvements in both adherence and blood pressure control.
Case Description
A 52-year-old male with long-standing hypertension (BP 170/100 mmHg) presented repeatedly to the ED despite being on triple antihypertensive therapy. The patient reported anxiety surrounding medication side effects, and disclosed compulsive pill-counting, hoarding, and dose-skipping behaviors, especially if routines were disrupted. Psychiatric evaluation revealed previously undiagnosed OCD (Y-BOCS score 28), primarily centered on contamination fears. He underwent 12 weeks of structured ERP therapy focusing on medication-related rituals. Following treatment, his BP decreased to 128/82 mmHg, and medication adherence improved to 100%, confirmed through pill counts and electronic monitors. Emergency room visits dropped from six per year to zero.
Discussion
This case underscores how OCD can present as “compulsive non-adherence,” where rituals—rather than deliberate refusal—drive treatment failure. Traditional adherence strategies (education, reminders) would likely have failed in this case. Instead, ERP successfully disrupted the OCD cycle, resolving the core behavioral barrier to adherence. This case reframes nonadherence not as defiance but as a psychiatric symptom, demanding psychiatric solutions. It advocates for routine mental health screening in patients with apparent treatment-resistant conditions and highlights the critical role of behavioral cardiology in managing chronic disease. Recognizing psychological drivers of nonadherence can lead to transformative improvements in both physiological outcomes and quality of life.
More abstracts on this topic:
A cerebrovascular longitudinal atlas: different rates of morphological change in aneurysm patients associated with hypertension and diabetes
Chien Aichi, Salamon Noriko, Vinuela Fernando, Szeder Viktor, Colby Geoffrey, Jahan Reza, Boyle Noel, Villablanca Juan, Duckwiler Gary
A closed-loop system based on piezoelectric thin-film sensors and photothermal nanomaterials enables precise renal denervation for the treatment of hypertensionLiu Chengzhe, Zhou Liping, Yu Lilei