Final ID: MP1585
Oral anticoagulant use in patients with atrial fibrillation post-catheter ablation: A retrospective analysis of a US commercial insurance database
Abstract Body (Do not enter title and authors here): Introduction: Catheter ablation is an effective strategy for the maintenance of sinus rhythm and enhancement of quality of life in patients with atrial fibrillation (AF). Oral anticoagulants (OAC) are recommended for at least 3 months post-ablation and indefinitely in patients with CHA2DS2-VASc score ≥2.
Research Question: What is the pattern of OAC use from the time of ablation to one year after ablation with respect to CHA2DS2-VASc score?
Methods: Patients with AF who underwent ablation (index date) from Jan 2017 to Oct 2023 were identified from Optum Clinformatics EDM–DoD. The cohort was divided into three groups: CHA2DS2-VASc 0 (low risk), 1 (intermediate risk), and ≥ 2 (high risk). Additionally, a subgroup with score ≥ 4 (very high-risk) was assessed. Treatment with OACs (i.e., direct oral anticoagulants or vitamin K antagonists) was assessed within the 30-day window following the ablation and at 1-year.
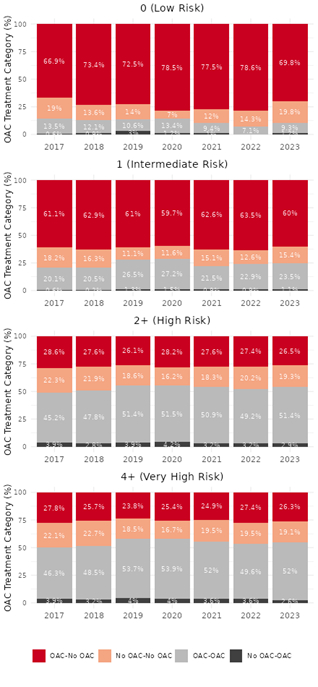
Results: Patients with CHA2DS2-VASc scores 0, 1, and ≥ 2 accounted for 2.8%, 7.5%, and 89.7% of the total population, respectively, with the ≥ 4 subgroup accounting for 61.6% of the total. The mean (SD) age was 52 (9), 58 (9), 70 (8), and 72 (7) years with females accounting for 0%, 14%, 42%, and 48% respectively. Many medical conditions were prevalent including hypertension (86%), obesity (45%), heart failure (44%), sleep apnea (41%), chronic kidney disease (25%) and diabetes (21%). For the low-risk group, OAC discontinuation ranged 66.9 to-78.6% at 1-year, and OAC continuation decreased by ~ 4% from 13.5% to 9.3% between 2017 and 2023. For patients in the intermediate risk group, OAC discontinuation was stable (~ 60%) and the continued use of OAC in the 1-year period increased by ~ 3% from 20.1% to 23.5%. For patients in the high-risk group, OAC discontinuation decreased by ~ 2% from 28.6% to 26.5% and the continued use of OAC increased by ~ 6% from 45.2% to 51.4%. For patients in the very high-risk group, OAC discontinuation minimally decreased, and OAC continuation increased by ~5% from 46.3% to 52%. In a stable minority of patients (~10-20%) across all risk groups, OAC was not used at the time of ablation or after. (Figure 1)
Conclusion: Patterns of OAC treatment following AF ablation were variable across CHA2DS2-VASc score subgroups. The discordance between guideline recommendations and clinical practice with respect to post-AF ablation OAC use may have an important impact on cardiovascular outcomes.
Research Question: What is the pattern of OAC use from the time of ablation to one year after ablation with respect to CHA2DS2-VASc score?
Methods: Patients with AF who underwent ablation (index date) from Jan 2017 to Oct 2023 were identified from Optum Clinformatics EDM–DoD. The cohort was divided into three groups: CHA2DS2-VASc 0 (low risk), 1 (intermediate risk), and ≥ 2 (high risk). Additionally, a subgroup with score ≥ 4 (very high-risk) was assessed. Treatment with OACs (i.e., direct oral anticoagulants or vitamin K antagonists) was assessed within the 30-day window following the ablation and at 1-year.
Results: Patients with CHA2DS2-VASc scores 0, 1, and ≥ 2 accounted for 2.8%, 7.5%, and 89.7% of the total population, respectively, with the ≥ 4 subgroup accounting for 61.6% of the total. The mean (SD) age was 52 (9), 58 (9), 70 (8), and 72 (7) years with females accounting for 0%, 14%, 42%, and 48% respectively. Many medical conditions were prevalent including hypertension (86%), obesity (45%), heart failure (44%), sleep apnea (41%), chronic kidney disease (25%) and diabetes (21%). For the low-risk group, OAC discontinuation ranged 66.9 to-78.6% at 1-year, and OAC continuation decreased by ~ 4% from 13.5% to 9.3% between 2017 and 2023. For patients in the intermediate risk group, OAC discontinuation was stable (~ 60%) and the continued use of OAC in the 1-year period increased by ~ 3% from 20.1% to 23.5%. For patients in the high-risk group, OAC discontinuation decreased by ~ 2% from 28.6% to 26.5% and the continued use of OAC increased by ~ 6% from 45.2% to 51.4%. For patients in the very high-risk group, OAC discontinuation minimally decreased, and OAC continuation increased by ~5% from 46.3% to 52%. In a stable minority of patients (~10-20%) across all risk groups, OAC was not used at the time of ablation or after. (Figure 1)
Conclusion: Patterns of OAC treatment following AF ablation were variable across CHA2DS2-VASc score subgroups. The discordance between guideline recommendations and clinical practice with respect to post-AF ablation OAC use may have an important impact on cardiovascular outcomes.
More abstracts on this topic:
Association of Biomarkers with risk of Hematoma Expansion and Arterial Thromboembolic Events in Acute Factor Xa Inhibitor-Associated Intracerebral Hemorrhage: The ANNEXa-I Biomarker Substudy
Shoamanesh Ashkan, Verhamme Peter, Eikelboom John, Sharma Mukul, Xu Lizhen, Bamberg Krister, Beyer-westendorf Jan, Falkenberg Cecilia, Ladenvall Per, Narayan Rohit, Penland Robert
A comparison of the efficacy of initial high energy versus initial low energy biphasic shocks for cardioversion of atrial fibrillation and atrial flutter – a real-life experienceAlampoondi Venkataramanan Sai Vikram, Vunnam Ramarao, Voruganti Dinesh, Tsai Shane