Final ID: MDP29
Exploring mediation through major bleeding between direct oral anticoagulants and cardiovascular (CV) events
Abstract Body (Do not enter title and authors here): Introduction
Although extracranial major bleeding (EMB) is often transient and manageable with supportive care, there is concern that EMB may have a subsequent detrimental effect on CV outcomes. However, a causal relationship is unclear, because the association is often confounded by underlying disease and comorbidities. Clinical trial data for more comprehensive analyses via advanced modeling are limited.
Research Question
What is the effect of rivaroxaban vs. warfarin on CV outcomes mediated through EMB?
Aim
To determine the extent of the effect of rivaroxaban vs. warfarin on CV outcomes that is mediated through their differential impact on EMB using a novel, advanced modeling approach (EUPAS1000000168).
Methods
Using 5 US observational databases from routine clinical practice (01-11-2010 to 31-12-2022), adult patients with non-valvular atrial fibrillation (NVAF) were identified to establish the target and comparator cohorts, with 1st exposure as index date. Treatment balance was achieved by matching on propensity scores derived from large-scale regularized regression. Cox proportional hazards models estimated the main effect on CV outcomes (myocardial infarction, ischemic stroke, and composite endpoint) for rivaroxaban vs warfarin, with target and comparator time-at-risk right-censored at therapy end or switch, event occurrence, or database observation end. The EMB mediation effect on outcomes was estimated by including EMB as time-varying covariate, while controlling mediator-outcome confounding by including a mediator risk score in the outcome model. Comparative analyses were conducted only when pre-specified diagnostics passed for covariate balance, equipoise, and systematic error estimated through negative controls.
Results
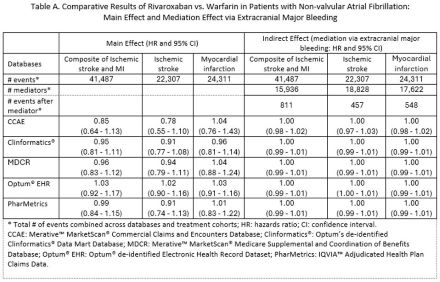
In 5 databases, 378,384 rivaroxaban initiators were matched to 601,174 warfarin initiators with NVAF. Common comorbidities included hypertension, hyperlipidemia, coronary artery disease, and heart failure. Main effects and indirect effects (mediation effects) are in Table A.
Conclusion
This analysis suggested that EMB had no impact on the effect of rivaroxaban vs. warfarin on CV outcomes. A limitation is that EMB occurrence and CV events after EMB were limited, which reduced mediation impact.
Although extracranial major bleeding (EMB) is often transient and manageable with supportive care, there is concern that EMB may have a subsequent detrimental effect on CV outcomes. However, a causal relationship is unclear, because the association is often confounded by underlying disease and comorbidities. Clinical trial data for more comprehensive analyses via advanced modeling are limited.
Research Question
What is the effect of rivaroxaban vs. warfarin on CV outcomes mediated through EMB?
Aim
To determine the extent of the effect of rivaroxaban vs. warfarin on CV outcomes that is mediated through their differential impact on EMB using a novel, advanced modeling approach (EUPAS1000000168).
Methods
Using 5 US observational databases from routine clinical practice (01-11-2010 to 31-12-2022), adult patients with non-valvular atrial fibrillation (NVAF) were identified to establish the target and comparator cohorts, with 1st exposure as index date. Treatment balance was achieved by matching on propensity scores derived from large-scale regularized regression. Cox proportional hazards models estimated the main effect on CV outcomes (myocardial infarction, ischemic stroke, and composite endpoint) for rivaroxaban vs warfarin, with target and comparator time-at-risk right-censored at therapy end or switch, event occurrence, or database observation end. The EMB mediation effect on outcomes was estimated by including EMB as time-varying covariate, while controlling mediator-outcome confounding by including a mediator risk score in the outcome model. Comparative analyses were conducted only when pre-specified diagnostics passed for covariate balance, equipoise, and systematic error estimated through negative controls.
Results
In 5 databases, 378,384 rivaroxaban initiators were matched to 601,174 warfarin initiators with NVAF. Common comorbidities included hypertension, hyperlipidemia, coronary artery disease, and heart failure. Main effects and indirect effects (mediation effects) are in Table A.
Conclusion
This analysis suggested that EMB had no impact on the effect of rivaroxaban vs. warfarin on CV outcomes. A limitation is that EMB occurrence and CV events after EMB were limited, which reduced mediation impact.
More abstracts on this topic:
Characterization of Acute Ischemic Stroke (AIS) patients excluded from thrombolysis due to recent NOAC use.
Mok Kent, Palmisano Caitlin, Mcardle Patrick, Mehndiratta Prachi, Chaturvedi Seemant
A Blood(y) Pressure Crisis: Diffuse Alveolar Hemorrhage as a Rare Manifestation of Severely Uncontrolled HypertensionNandyal Shreyas, Amdetsion Gedion Yilma, Varma Revati, Kohli Saksham, Hammo Hasan