Final ID: 4359746
Safety and Feasibility of Hyperkalemic Cardioplegia with Diazoxide in Cardiac Surgery: CPG-DZX Trial
Abstract Body (Do not enter title and authors here): Introduction
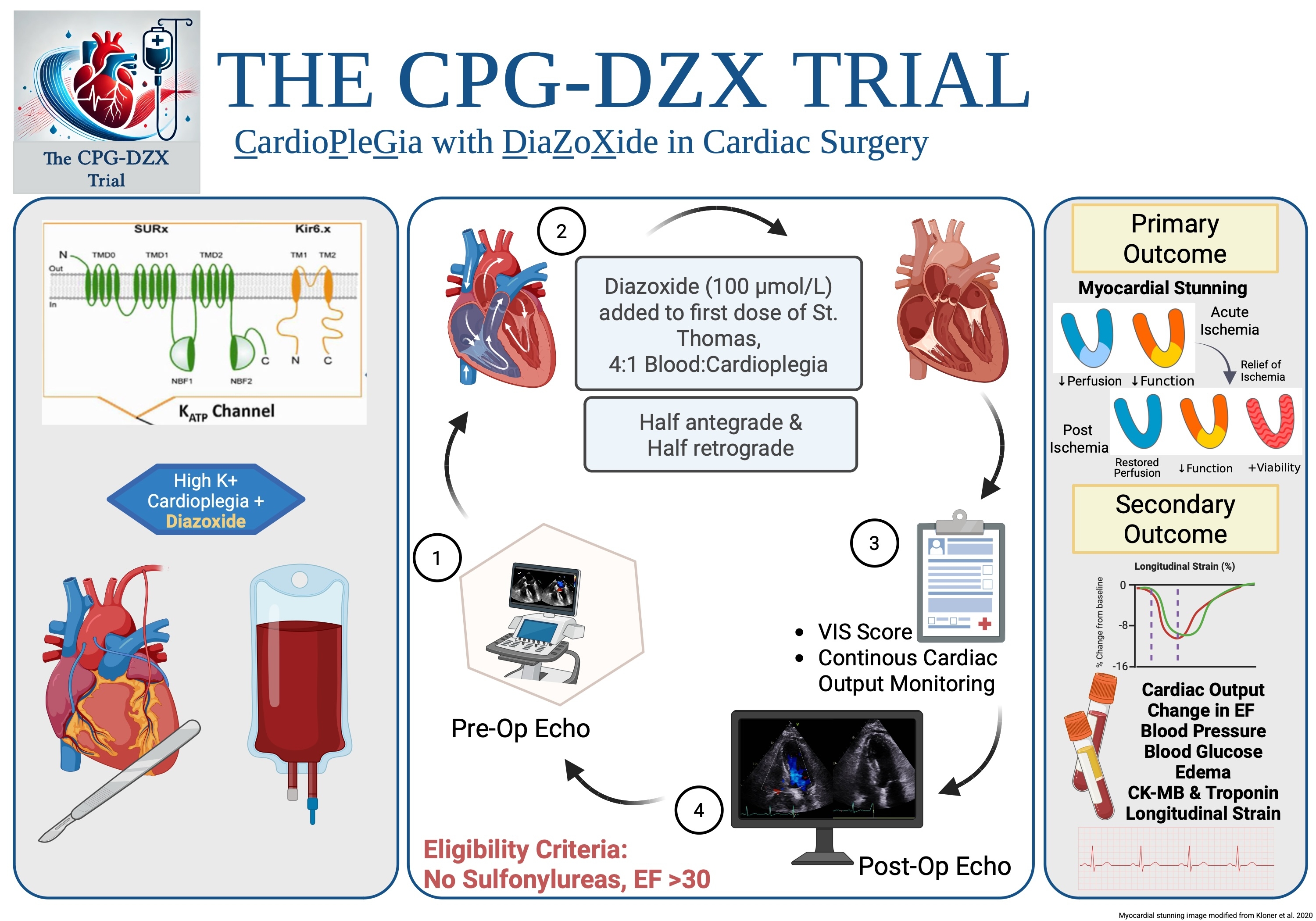
Adenosine triphosphate-sensitive potassium (KATP) channel opener diazoxide (DZX) is cardioprotective in multiple translational animal models. We report the first in human FDA approved Phase I safety and feasibility trial of diazoxide in hypothermic hyperkalemic cardioplegia in patients undergoing cardiac surgery. The aim of this study was to demonstrate the safety and feasibility of DZX in patients undergoing cardiac surgery. The results will support a future Phase III randomized controlled trial to evaluate stunning in patients after cardiac surgery with DZX.
Hypothesis
We hypothesize that DZX can be safely administered in hypothermic hyperkalemic cardioplegia in cardiac surgery.
Methods
Patients undergoing non-emergent cardiac surgery (coronary artery bypass, aortic, or valve) received 100 microM/L intracoronary DZX delivered in the first dose of hypothermic, hyperkalemic cardioplegia at the time of cross-clamp placement. Patients on KATP channel inhibitors or with left ventricular ejection fraction (LVEF) <30% were excluded. Primary safety endpoints were changes in blood glucose, mean arterial pressure (MAP), and weight gain. Additional data collected included the presence of myocardial stunning (using a novel definition of the need for mechanical and/or inotropic support >24 and <72 hours), the difference in pre- and postoperative LVEF, and time to wean from bypass.
Results
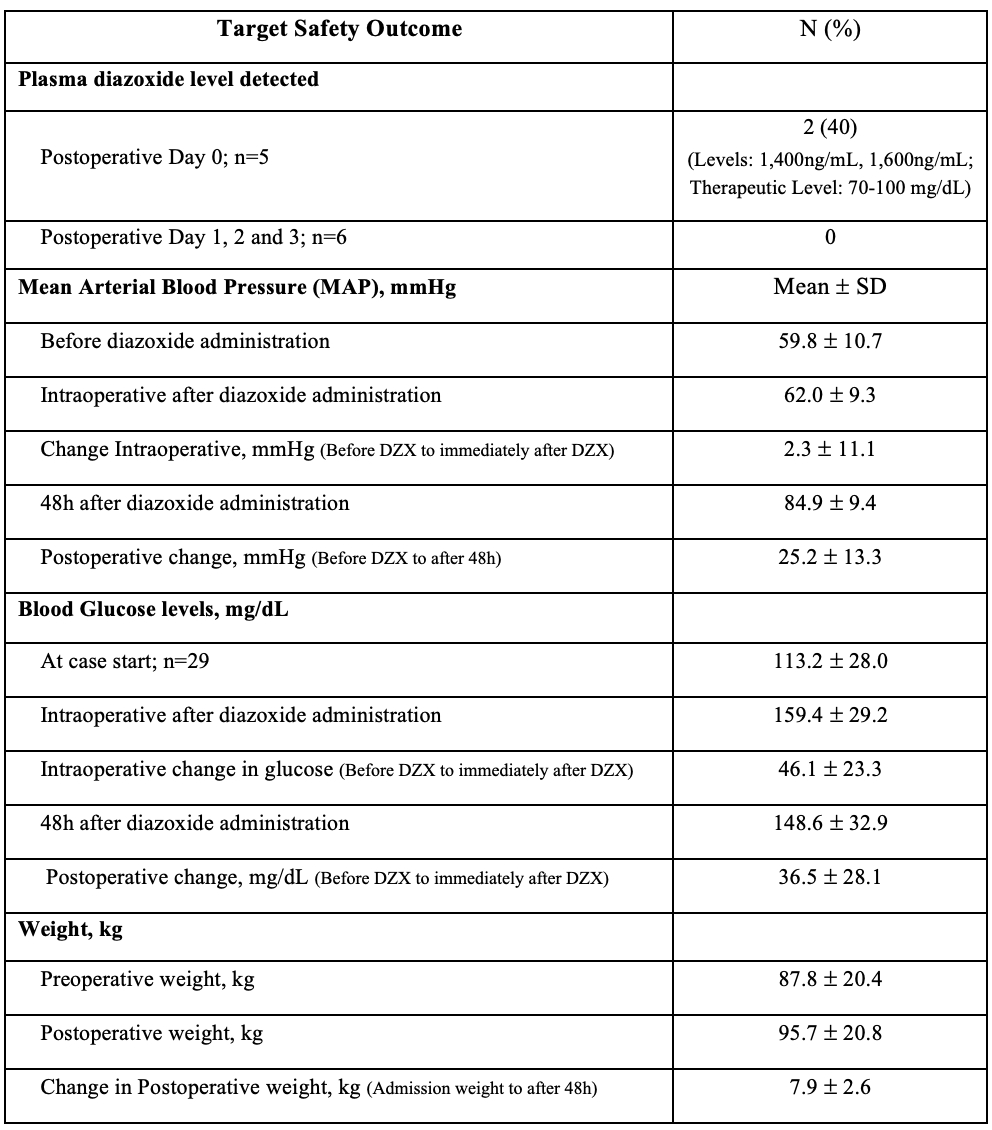
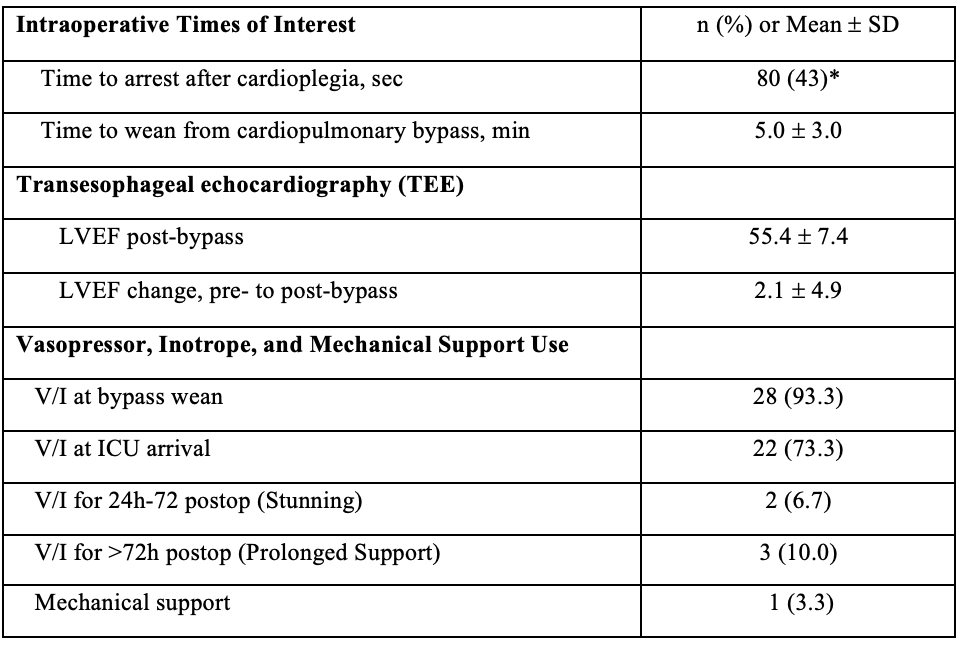
Thirty patients received intracoronary DZX. One serious adverse event occurred, unrelated to DZX. The mean MAPs before DZX were 59.8 mmHg (last intraoperative MAP before DZX) and 62.0 mmHg (lowest MAP within 5 min after DZX). Intraoperative glucose before DZX was a mean of 113 mg/dL (at case start) and a mean of 159 mg/dL after DZX (point-of-care, intraoperative). Patients gained a mean of 7.9 kg postoperatively (preoperative weight compared to 48-hr postoperative) (Table 1). In the first 12 hrs postoperatively, mean peak lactate was 5.6±5.1 and peak troponin was 12,531±18,615 ng/L. Two patients (6.7%) had stunning. Intraoperative transesophageal echocardiography (TEE) pre- and post-bypass showed that mean LVEF significantly increased from baseline (2.1±4.9%, p=0.024). Mean time to cardiac arrest was 80±44 seconds, and time to wean from bypass was 5±3 min (Table 2).
Conclusion
Intracoronary DZX can be safely administered in hypothermic hyperkalemic cardioplegia in cardiac surgery.
Adenosine triphosphate-sensitive potassium (KATP) channel opener diazoxide (DZX) is cardioprotective in multiple translational animal models. We report the first in human FDA approved Phase I safety and feasibility trial of diazoxide in hypothermic hyperkalemic cardioplegia in patients undergoing cardiac surgery. The aim of this study was to demonstrate the safety and feasibility of DZX in patients undergoing cardiac surgery. The results will support a future Phase III randomized controlled trial to evaluate stunning in patients after cardiac surgery with DZX.
Hypothesis
We hypothesize that DZX can be safely administered in hypothermic hyperkalemic cardioplegia in cardiac surgery.
Methods
Patients undergoing non-emergent cardiac surgery (coronary artery bypass, aortic, or valve) received 100 microM/L intracoronary DZX delivered in the first dose of hypothermic, hyperkalemic cardioplegia at the time of cross-clamp placement. Patients on KATP channel inhibitors or with left ventricular ejection fraction (LVEF) <30% were excluded. Primary safety endpoints were changes in blood glucose, mean arterial pressure (MAP), and weight gain. Additional data collected included the presence of myocardial stunning (using a novel definition of the need for mechanical and/or inotropic support >24 and <72 hours), the difference in pre- and postoperative LVEF, and time to wean from bypass.
Results
Thirty patients received intracoronary DZX. One serious adverse event occurred, unrelated to DZX. The mean MAPs before DZX were 59.8 mmHg (last intraoperative MAP before DZX) and 62.0 mmHg (lowest MAP within 5 min after DZX). Intraoperative glucose before DZX was a mean of 113 mg/dL (at case start) and a mean of 159 mg/dL after DZX (point-of-care, intraoperative). Patients gained a mean of 7.9 kg postoperatively (preoperative weight compared to 48-hr postoperative) (Table 1). In the first 12 hrs postoperatively, mean peak lactate was 5.6±5.1 and peak troponin was 12,531±18,615 ng/L. Two patients (6.7%) had stunning. Intraoperative transesophageal echocardiography (TEE) pre- and post-bypass showed that mean LVEF significantly increased from baseline (2.1±4.9%, p=0.024). Mean time to cardiac arrest was 80±44 seconds, and time to wean from bypass was 5±3 min (Table 2).
Conclusion
Intracoronary DZX can be safely administered in hypothermic hyperkalemic cardioplegia in cardiac surgery.
More abstracts on this topic:
A novel reproducible low-cost model of acute myocardial infarction in swine
Li Yichen, Zheng Zilong, Tang Weijie, Chen Wangping, Yang Jinfu, Fan Chengming
Stroke Volume Work Index from speckle tracking is associated with mortality in critically ill patients with sepsis and septic shock.Lanspa Michael, Shvilkina Tatyana, Wiley Brandon, Dugar Siddharth, Sanchez Pablo, Hirshberg Eliotte, Graham Jeffrey, Grissom Colin, Brown Samuel