Final ID: MP1559
Underutilization of guideline-directed medical therapy following hospitalizations for heart failure with reduced ejection fraction among U.S. Veterans, 2022 to 2023
Abstract Body (Do not enter title and authors here): Background
Hospitalizations for heart failure with reduced ejection fraction (HFrEF) represent key opportunities to optimize guideline-directed medical therapy (GDMT). We sought to determine contemporary GDMT prescribing patterns following HFrEF hospitalization in the Veterans Health Administration (VA).
Methods
National retrospective cohort study of electronic health records from VA. We included adults hospitalized with a primary diagnosis of HFrEF between 2022-2023 who were discharged home. Optimal GDMT was defined as treatment with four classes (beta-blockers, BB, renin-angiotensin-aldosterone system inhibitors, RAASi, mineralocorticoid receptor antagonists, MRA, and sodium glucose-like transporter 2 inhibitors, SGLT2i). We identified GDMT present on admission and GDMT initiated in hospital or within 7 days of discharge to determine (1) if the number of GDMT classes was intensified and (2) if optimal GDMT was received. Among those admitted on suboptimal GDMT, we used multivariable logistic regression to examine the association of five key sociodemographic domains (age, sex, race and ethnicity, rurality, and neighborhood resource deprivation) with GDMT use controlling for clinical and facility-level factors.
Results
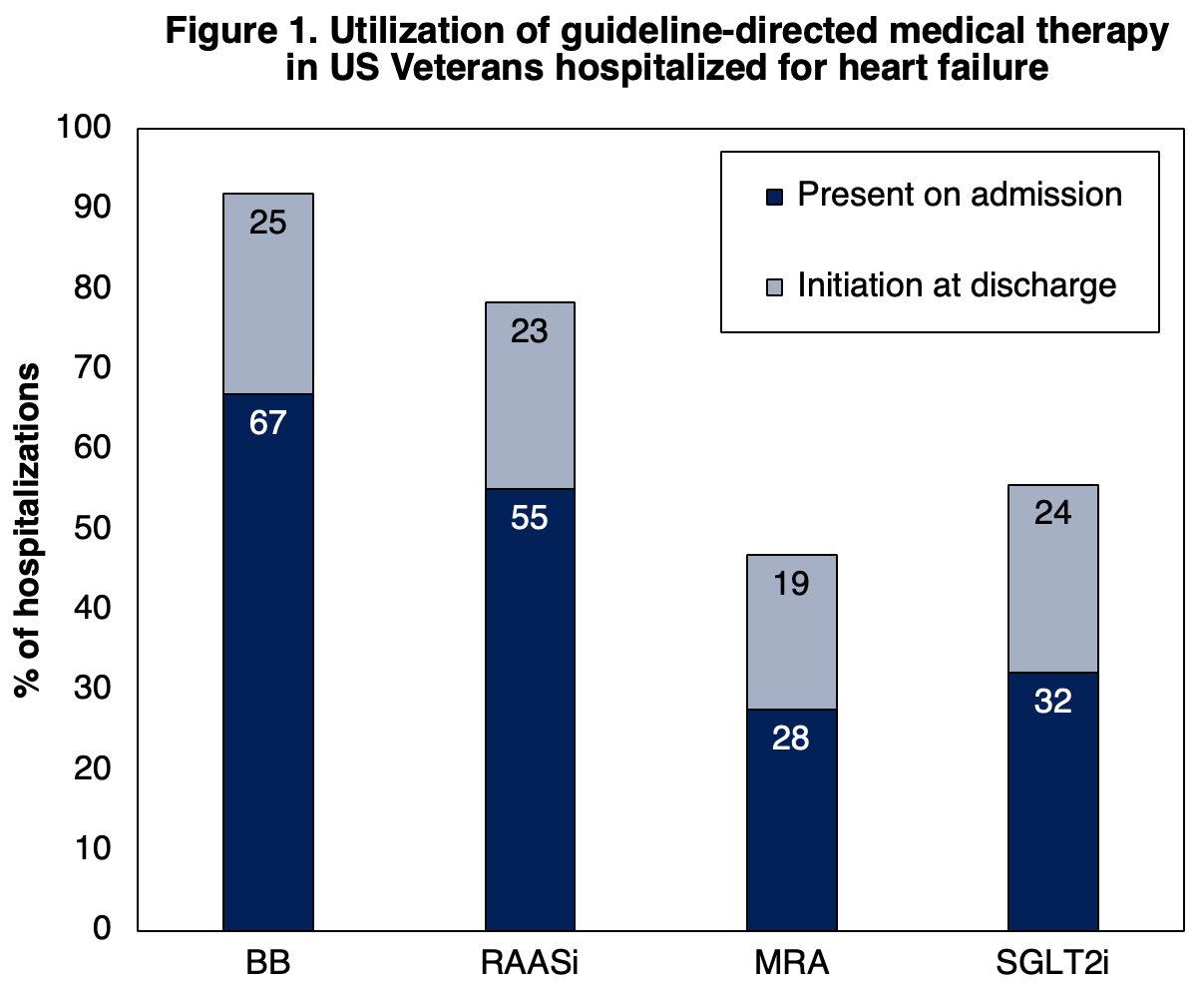
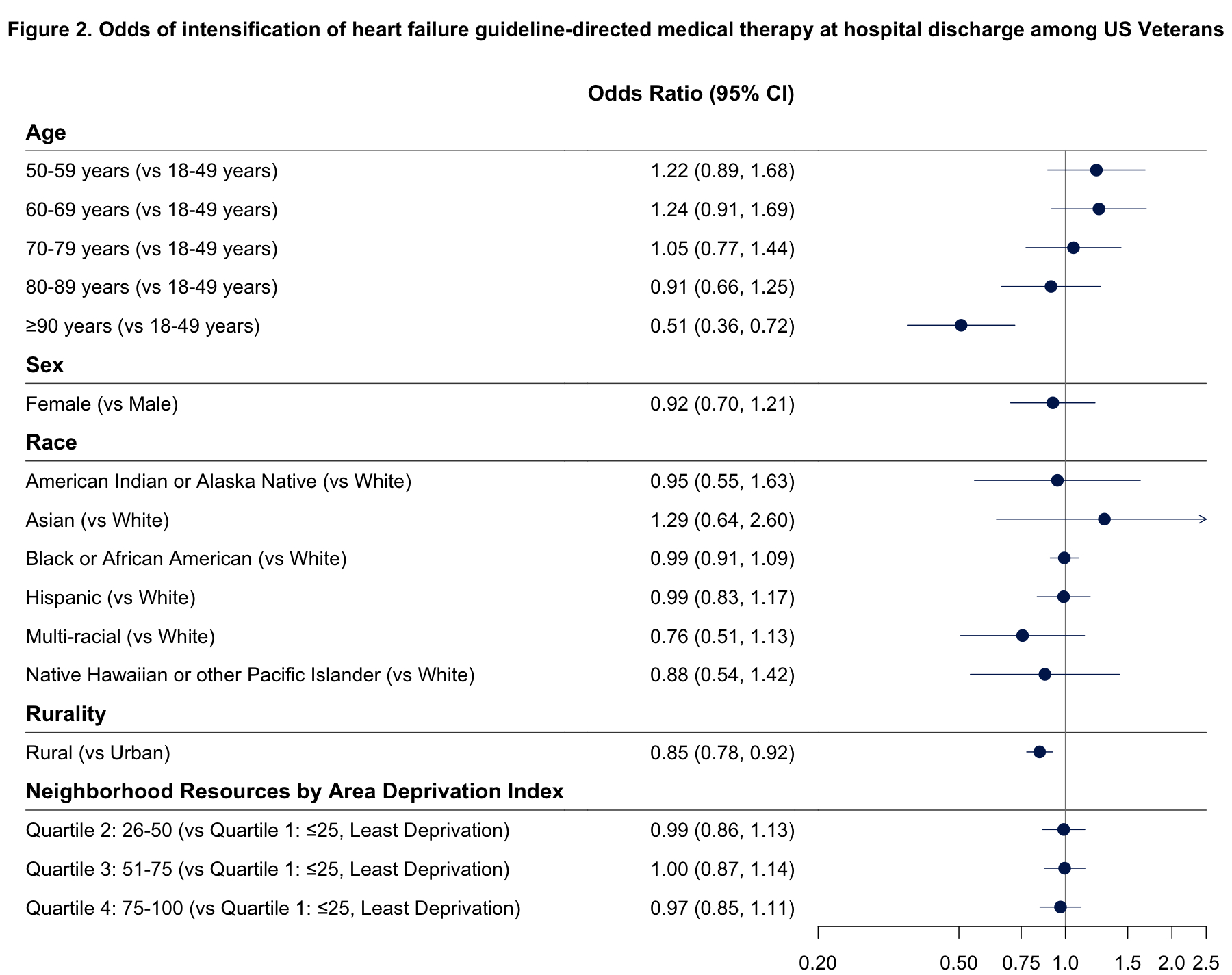
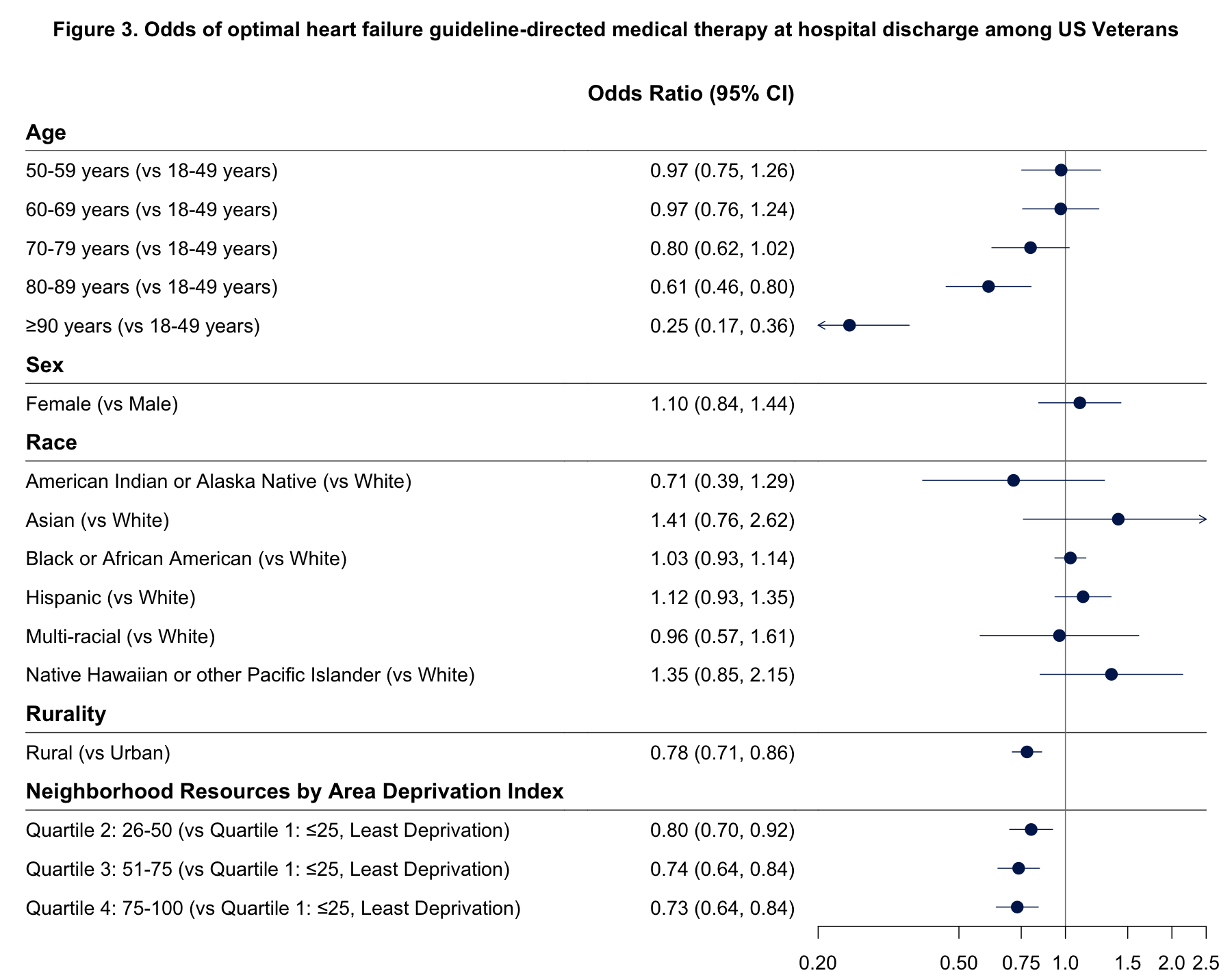
The cohort included 20,866 HFrEF hospitalizations (60% aged ≥70 years, 2% female, 48% White, 38% Black, 39% rural). The proportion of patients on optimal GDMT increased from 12% on admission to 29% on discharge. Of those on suboptimal GDMT on admission, 56% intensified GDMT and 29% initiated ≥2 new GDMT classes. At admission, 67%, 55%, 28%, and 32% were using BBs, RAASis, MRAs, and SGLT2is, respectively (Figure 1). At discharge, GDMT use increased to a total of 92%, 78%, 47%, and 56%, respectively. Older patients were less likely to intensify GDMT (Figure 2) or receive optimal GDMT (Figure 3) at discharge. There were no differences in GDMT use by sex, race or ethnicity. Patients residing in rural areas were less likely to receive GDMT intensification (OR: 0.86; 95% CI, 0.78 to 0.92) and optimization (OR: 0.78; 95% CI, 0.71 to 0.86). Patients living in neighborhoods with fewer resources were less likely to receive optimal GDMT, but had similar rates of GDMT intensification.
Conclusions
Among Veterans hospitalized for HFrEF only a third received optimal GDMT while over half intensified GDMT at discharge. Disparities in GDMT initiation at discharge by age, rurality, and neighborhood highlight opportunities for targeted quality improvement efforts.
Hospitalizations for heart failure with reduced ejection fraction (HFrEF) represent key opportunities to optimize guideline-directed medical therapy (GDMT). We sought to determine contemporary GDMT prescribing patterns following HFrEF hospitalization in the Veterans Health Administration (VA).
Methods
National retrospective cohort study of electronic health records from VA. We included adults hospitalized with a primary diagnosis of HFrEF between 2022-2023 who were discharged home. Optimal GDMT was defined as treatment with four classes (beta-blockers, BB, renin-angiotensin-aldosterone system inhibitors, RAASi, mineralocorticoid receptor antagonists, MRA, and sodium glucose-like transporter 2 inhibitors, SGLT2i). We identified GDMT present on admission and GDMT initiated in hospital or within 7 days of discharge to determine (1) if the number of GDMT classes was intensified and (2) if optimal GDMT was received. Among those admitted on suboptimal GDMT, we used multivariable logistic regression to examine the association of five key sociodemographic domains (age, sex, race and ethnicity, rurality, and neighborhood resource deprivation) with GDMT use controlling for clinical and facility-level factors.
Results
The cohort included 20,866 HFrEF hospitalizations (60% aged ≥70 years, 2% female, 48% White, 38% Black, 39% rural). The proportion of patients on optimal GDMT increased from 12% on admission to 29% on discharge. Of those on suboptimal GDMT on admission, 56% intensified GDMT and 29% initiated ≥2 new GDMT classes. At admission, 67%, 55%, 28%, and 32% were using BBs, RAASis, MRAs, and SGLT2is, respectively (Figure 1). At discharge, GDMT use increased to a total of 92%, 78%, 47%, and 56%, respectively. Older patients were less likely to intensify GDMT (Figure 2) or receive optimal GDMT (Figure 3) at discharge. There were no differences in GDMT use by sex, race or ethnicity. Patients residing in rural areas were less likely to receive GDMT intensification (OR: 0.86; 95% CI, 0.78 to 0.92) and optimization (OR: 0.78; 95% CI, 0.71 to 0.86). Patients living in neighborhoods with fewer resources were less likely to receive optimal GDMT, but had similar rates of GDMT intensification.
Conclusions
Among Veterans hospitalized for HFrEF only a third received optimal GDMT while over half intensified GDMT at discharge. Disparities in GDMT initiation at discharge by age, rurality, and neighborhood highlight opportunities for targeted quality improvement efforts.
More abstracts on this topic:
A Review Of The Burden, Management And Outcomes Of Patients With Aldosterone Dysregulation
Luan Shan, Agiro Abiy, Daniel Ian, Mckendrick Jan, Davis Harrison, Huang Joanna, Linganathan Karthik
A community-engaged approach to culturally tailoring a dietary intervention to improve cardiometabolic health among Black adults with obesity in Los Angeles CountyAdeyemo Mopelola, Thorpe Roland